The Pharmacist's Dos and Don'ts of Post-Intubation Sedation
Steph’s Note: This post is for all of you who have wondered what happens after the happily ever after of a movie. Sure, rapid sequence intubation (RSI) gets all the glitz and glamor of the critical care world, much like an anticipated smooch at the end of a rom-com. But what comes NEXT?
Don’t worry, we’ve got you covered. No need to write your own pharmacy fan fic. Tricia Dieso is here to illuminate us all! Dr. Dieso worked 4 years as a pharmacy technician at The Johns Hopkins Hospital and continued another 4 years as a pharmacy student while obtaining her pharmacy degree from Notre Dame of Maryland University. She graduated in May 2019 and headed to Grand Rapids, Michigan to pursue her PGY-1. She’s worked as an Emergency Medicine/Critical Care Pharmacist since finishing her residency. Cheers, and let’s get started!
So you've just intubated your patient, and now you are likely wondering a few things…
How long do I have before the induction agent wears off and my patient needs further sedation?
What agent do I use for sedation?
Is awake paralysis really a thing?
If any of these questions have crossed your mind or maybe you just want a refresher on post-intubation sedation, then this post is for you!
A (VERY) Quick Refresher on Rapid Sequence Intubation (RSI)
(Image)
Before we can answer those questions, let's take a quick look back at the induction and paralytic agents used for RSI. If this is too quick (like how Roadrunner zooms past Wile E. Coyote), check out our previous post or our cheatsheet on RSI for all the deets.
Here are those agents:
Like I said, a quick look. The main area I want you to focus on with these agents is the duration of action. That's where the meat and potatoes of this post today comes into play, so keep this in mind for when we get to the agents for continuous sedation.
How is Sedation Assessed?
Well, no, not this “Richmond.” But if you haven’t seen The IT Crowd, you should definitely check it out. (Image)
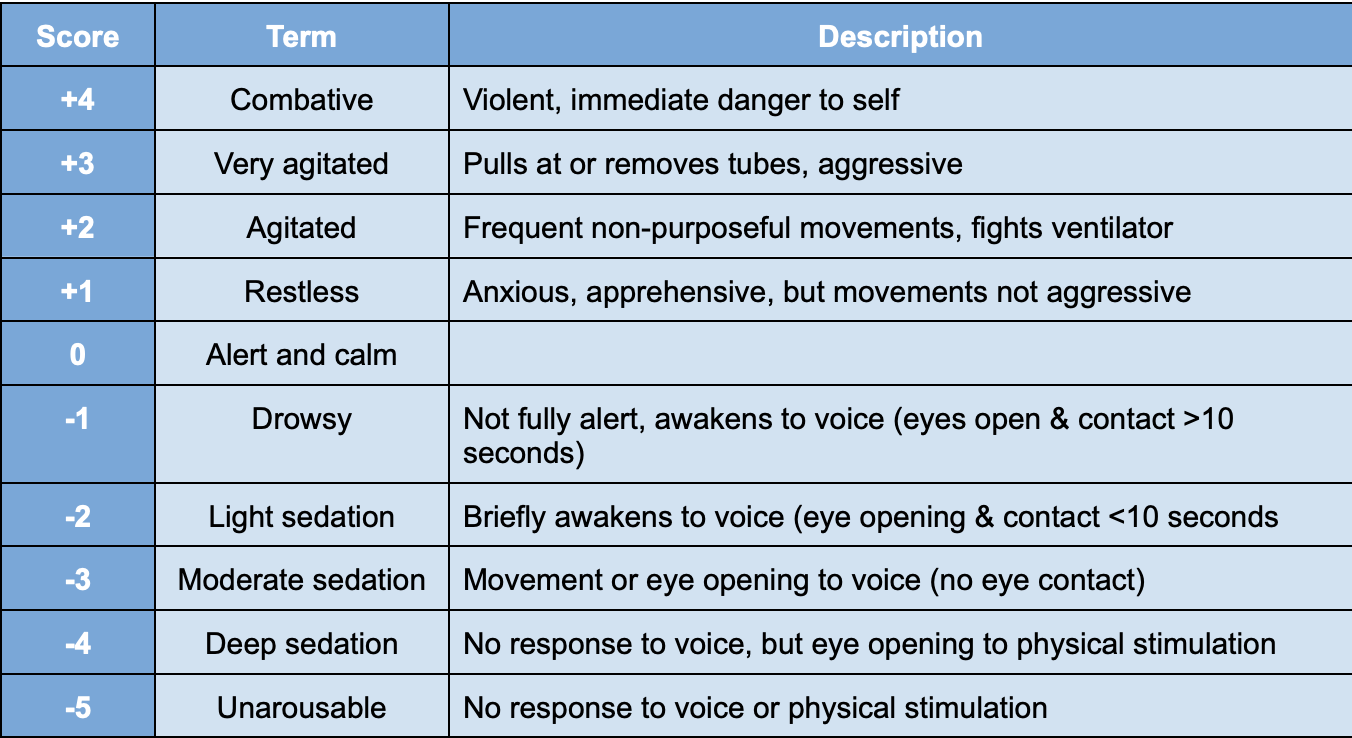
When seeking to sedate a patient after intubation, it’s important to first determine what Richmond Agitation Sedation Scale (RASS) goal you want for them. (Like Stephen Covey says, “Begin with the end in mind.”) Setting this goal comes down to why the patient was intubated in the first place.
Were they hyperactive after a drug ingestion or unable to protect their airway due to a COPD exacerbation? Or maybe they were in anaphylaxis with a closing airway. If it was the first scenario, you likely want them more sedated than someone who was more calm prior to the intubation. Either way, it's important to understand what RASS goal you want. RASS ranges from a -5 to a +4, as you can see below:
The majority of the research out there today shows that having a RASS goal of 0 to -2 is desirable. Any sedation deeper than that can lead to your patient being intubated for longer. Now that being said, there may be reasons to have your patients in a deeper sedation… For example, perhaps they need to be paralyzed to aid in recovery, or their brain needs time to recover. But generally speaking, 0 to -2 is generally a solid goal range. Once you determine what your patient's personal goal is, you can then decide which sedative is ideal.
Pharmacologic Agents for Post-RSI Sedation
One thing I want to stress is that AWAKE PARALYSIS IS REAL! It’s essential to know which sedation agent was used during the induction phase of RSI because certain agents wear off before the paralytic. No bueno…
The easiest way to determine if a patient is experiencing awake paralysis is to monitor vital signs. Stress manifests as tachycardia and hypertension, and awake paralysis certainly seems like one of the most stressful situations I can imagine!
No one wants to be awake and alert to their surroundings but not able to move their body. (That sounds like the seventh circle of H-E-L-L, wouldn’t you agree?)
Of note, the issue of awake paralysis doesn't just come into play with post-intubation sedation. It’s also a consideration if your patient is on a continuous infusion paralytic and you want to wean sedation. You should fully wait for the paralytic to wear off before weaning sedation so as to save them this terrible feeling.
Ok, I think I have made my point clear. For now, let's move on to our options for sedation.
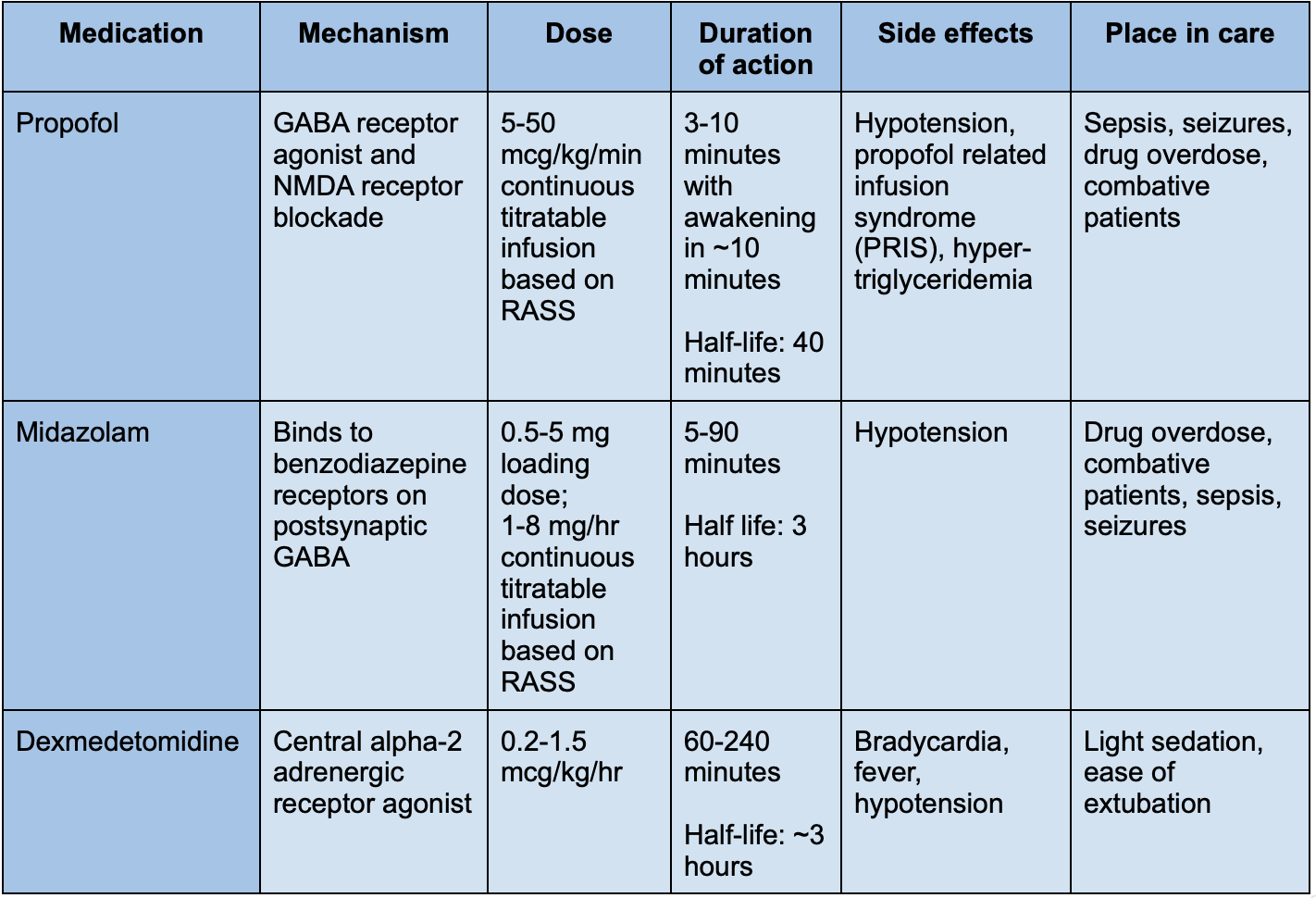
There are a few pearls to take away from this table:
Propofol is typically a great option for all indications. Monitor for hypotension, especially in septic patients. They may need vasopressor support.
Propofol can cause hypertriglyceridemia if used for an extended period of time. Be sure to monitor triglyceride levels.
Dexmedetomidine achieves, AT MAX, RASS -1 and does not deeply sedate patients. If a deeper sedation is needed, look to propofol or midazolam.
Dexmedetomidine is a great option to aid in extubating patients and help with re-emergence.
Pharmacologic Agents for Post-RSI Pain
Another essential area we pharmacists HAVE to consider post-intubation is pain. Think about it… The patient now has an endotracheal tube in place, and those things don’t always slide in smoothly on the first attempt like we see on TV. (Yeah, yikes!) No doubt that it's a weird feeling with some associated pain from insertion.
Thankfully, we have a couple options in our analgesic arsenal that can be used as either intermittent boluses or continuous infusions.
A couple pearls to take away from this table:
Fentanyl is typically the drug of choice in ventilated patients due to its shorter duration of action.
Opioids have no real maximum due to patients becoming tolerant. Consider switching to a different opioid if escalating doses do not provide adequate pain control.
The tl;dr of Post-RSI Sedation for Pharmacists
Post-intubation sedation is an important step after RSI has been performed because (as I have hopefully ingrained in your brain) awake paralyzation IS REAL! The ideal time to initiate continuous sedation after RSI all depends on which initial sedation medications were used, although it's best to have it all planned out prior to RSI being performed.
DO think of it as a mental check-list before even beginning RSI: sedation, paralytic, post sedation…check, check, and check!
DON’T forget to individualize a RASS goal for your patient based on the clinical scenario.
DO be sure to pick appropriate analgesia for your patient to accompany the sedation.
DON’T forget to wean the paralytic BEFORE weaning sedation!
Now you're ready to provide the best possible intubation experience for your patient. When in doubt, always ask yourself, "How would I feel if I was in their shoes?"