Biosimilars - A User Friendly Guide
If you’ve read any pharmacy news in the past couple of years, you’ve come across the term “biosimilar.”
Sure, you might just glaze over it when you’re scrolling through your daily ASHP/APhA/AMCP list serve email (has anyone else noticed that all of these publications are almost identical?). But no doubt you’ve seen it.
New biosimilar for Rituxan
New biosimilar for Neulasta
New biosimilar for Procrit
And then you start seeing multiple biosimilars to the same product (there are 3 for Neulasta and 5 for Herceptin at the time of this writing).
It’s enough to overwhelm even the most up to date practitioners.
That’s where tl;dr comes in. This post will teach you exactly what a biosimilar is, how they differ from reference products, limitations of their use, and more. Let’s dig in.
What is a Biologic?
Before I go all biosimilar on your ass, we need to understand what a biologic is.
Let’s start with the textbook definition of a biologic — A large, complex molecule synthesized through biotechnology in a living system.
That’s great and all, but it lacks some of the “poetic flair” that tl;dr is known for. Let’s look at the production process to gain a better understanding (and appreciation) for just how friggin cool this is.
The overall concept with biologics is that we turn a living cell into a production factory, and use it to make many copies of some protein. If this sounds familiar, it’s because viruses do the exact same thing when they infect one of your cells.
This is fundamentally different than how other “conventional” drugs are made. To make gabapentin, you just need to mix the right ingredients together with the right reagents in the right order. Put the resulting mixture inside of a capsule, and you’re golden.*
*I’m sure I just pissed off a lot of pharmaceutical chemists. Sorry! I know the process is more complicated than that…I’m just illustrating a point!
With a biologic, the process is slightly more complex. It involves sticking a piece of DNA inside of a cell (the production cell). This production cell could be bacteria, yeast, or it might be something weird like a Chinese Hamster Ovary.
Once the DNA is in the production cell, the production cell can produce whatever protein the DNA codes for. This protein is our molecule of interest…the “workhorse” of the biologic drug.
I’m making copies of an ANTIBODY!! (Image)
Then we give our beautiful Frankenstein production cell everything it needs to grow and thrive in this cruel and harsh world.
It divides and divides and divides until we have millions of identical copies. And these production cell clones keep churning out that same identical protein.
We process and clean up the resulting solution —making sure all that’s left is the molecule of interest (the protein). This isolated protein is the active ingredient of our new biologic.
Finally, we price it at $9,000 per vial, and our work is done.
(kidding, kidding…sort of. More on that later.)
What is a Biosimilar?
You might have guessed this from the name, but a biosimilar is “highly similar” to a biologic. Clever, no?
When talking about biosimilars, the original biologic is known as the reference product. The biosimilar has to meet a few criteria:
It must have the same mechanism of action
It must be administered the same way
Biologics (and therefore biosimilars) are usually given by parenteral injection since they are proteins and would be degraded in the stomach
It must have “no clinically meaningful differences” in terms of safety and efficacy from the reference product
There is a lot of testing that goes into meeting these criteria. There are extensive pharmacokinetic tests (looking at ADME — absorption, distribution, metabolism, and excretion). There are pharmacodynamic tests (looking at the time the molecule remains bound to the target receptor, and clinical response). Finally, we’re checking the immunogenicity of the biosimilar to make sure we’re not causing an untoward immune response.
The official term for all of this is the “Totality of Evidence.”
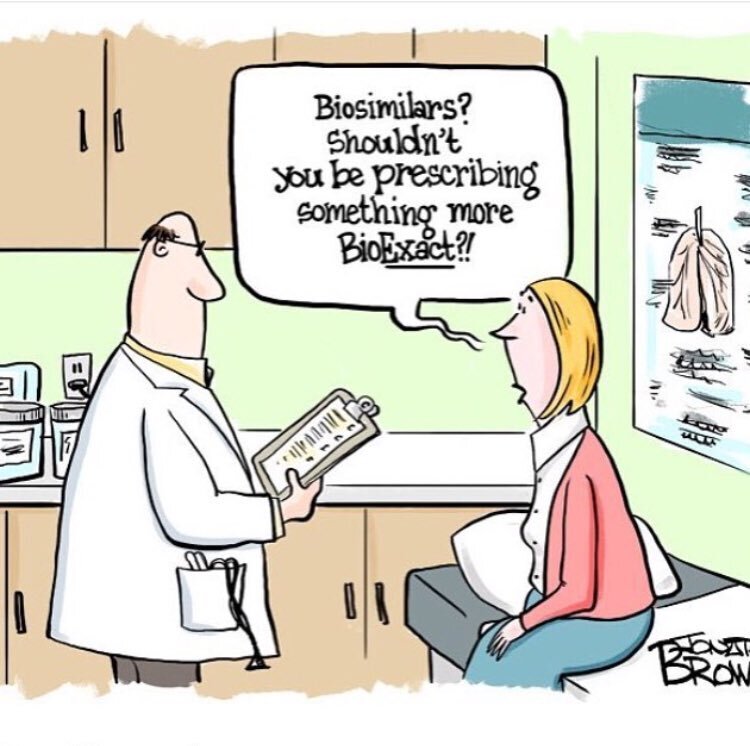
At this point, you might be thinking…
This sounds exactly like a generic drug…but for a biologic
—You, right now
BUT…you’d be wrong to think that.
There are a lot of parallels, and “generic” is a useful analogy for explaining what a biosimilar is to a patient. But, the fact remains: A biosimilar is NOT the same thing as a generic.
Here’s why…
Biosimilar vs Generic
There is some overlap between biosimilar drugs and generic drugs, but enough key differences to make them clinically (and, importantly, legally) distinct.
First, the similarities.
Both biosimilars and generics go through an abbreviated FDA approval pathway. This saves the manufacturers boatloads of money on clinical trials, allowing shorter time to market and (hopefully) less cost to the patient.
But — biosimilar drugs are…similar to the reference product.
They don’t necessarily need to be identical.
There’s a reason for this. Think back to the production process we outlined above. It would be damn near impossible to make a biosimilar that was identical to the reference product.
This is fundamentally different than with generic drugs. With a generic drug, the active ingredient must be the same (not “similar”). Your generic version of Lipitor 10 mg must contain exactly 10 mg of atorvastatin. NOT 10 mg of an “atorvastatin-like substance.”
There is a big practice ramification here. When a pharmacist is handed a prescription for Lipitor 10 mg, she can dispense the generic atorvastatin (unless the prescription says “Brand Only” or “Dispense as Written”). She can do this without contacting the prescriber.
By contrast, if I receive a prescription for Humira, I cannot dispense Amjevita.
I can contact the prescriber and say “Humira requires a prior auth per this patient’s insurance plan. Please write a new prescription for Amjevita or complete this 15-page packet of medical necessity paperwork and fax it over to BCBS.”
But until I get a new prescription (or a PA approval), that patient is going to be giving me the hairy eyeball from my waiting room.
Here is a nice breakdown looking at differences in the approval process between biosimilars and generics:
Notice how much weight is placed on Clinical Studies for a biologic (reference product)…compared to how much weight is placed on Clinical Studies for biosimilars. (Image)
And here’s a handy chart that highlights some other key differences between biosimilars and generics:
Bonus points for the typo on the title ;) Image
Take special note of the “Interchangeable” part of the above chart. There IS a legal pathway that exists for a biosimilar to become interchangeable with the reference product. When it does this, we’d call it an “Interchangeable Product.”
Just like with a generic drug, a pharmacist can receive a prescription for the brand name Reference Product, and dispense the Interchangeable Product without contacting the prescriber.
There’s just one small caveat with Interchangeable Products…
None have been approved by the FDA.
In order to jump from "biosimilar” to “interchangeable”, there is a whole lotta extra data required. And that costs money and time, which limits the upside if you’re a pharmaceutical company.
My prediction is that it will be a long time before I have to update this article to include the first Interchangeable biologic product.
Biosimilar Naming Convention
Now, let’s talk about how to name a biosimilar. Since a biosimilar is only similar to the reference product, we can’t just use the name of the reference product for our biosimilar.
But…we can’t make up a new name either. We need some way to denote that our product is biosimilar to the reference product.
The FDA’s fix to this problem is to add 4 nonsense letters to the reference product to denote each biosimilar.
What do I mean by 4 nonsense letters? I mean 4 letters “devoid of meaning.” Let me give you some examples.
Pegfilgrastim is a biologic reference product used to prevent febrile neutropenia. As of this writing (January 2020), it has 3 approved biosimilars:
Pegfilgrastim [Neulasta] — Reference Product
Pegfilgrastim-jmdb [Fulphila] — Biosimilar
Pegfilgrastim-cbqv [Udenyca] — Biosimilar
Pegfilgrastim-bmez [Ziextenzo] — Biosimilar
So, yeah. 4 nonsense letters (unless -cbqv is a secret code that I’m out of the loop on). Per the FDA, these letters cannot be an acronym or any discernible word. Just 4 random letters without any recognizable meaning.
Adding to the confusion, the FDA recently expanded this policy so that all new BIOLOGICS have 4 nonsense letters added to the name of the reference product.
For example, Cemiplimab-rwlc [Libtayo], a drug for certain types of skin cancer, is the reference product.
But it wears 4 nonsense letters like a badge of honor on its packaging.
This may seem confusing, but it helps to differentiate each biologic/biosimilar as a unique product. This is critical, as we are going to be seeing a lot of them in the future.
Since I’m sure there will be a NAPLEX question on this eventually, The Purple Book is where you can find additional information about biosimilars, including the yet-to-exist interchangeability. While we’re on the subject, let’s also remember that we have The Orange Book for non-biologic drugs and The Pink Book for vaccines.
And if seeing a drug named “fam-trastuzumab deruxtecan-nkxi” (no, that’s not a typo) makes you have a seizure, then check out our breakdown of monoclonal antibodies. It may help ;)
Biosimilars and Extrapolation of Indication
Here’s a fun fact you may not know:
A biosimilar can be approved for an indication for which it’s never been studied.
Yes, you read that right. Let’s use an example to illustrate what I’m talking about…
Epoetin alfa [Procrit, Epogen] is a biologic used to increase red blood cell production and treat some types of anemia. It’s a reference product and has been studied in everything from anemia due to chronic kidney disease, chemo-induced anemia, myelodysplastic syndrome, and more. Epoetin alfa has shown benefit in all of these indications (some more than others) and is used regularly.
Epoetin alfa-epbx [Retacrit]is a biosimilar. It is approved for all of the same indications as Procrit. You can use it for any situation where you would use epoetin alfa.
But Retacrit has only been studied in patients with anemia due to chronic kidney disease.
It wasn’t studied in chemotherapy-induced anemia, zidovudine-induced anemia, or anything else on the Procrit package insert.
Going a step further, in the trials that led to Retacrit’s approval, all patients were initiated on Procrit (the reference product) and then switched to Retacrit. There isn’t any data for patients who start with Retacrit from scratch.
This is because biosimilars can extrapolate the indications of their reference product. If it shows similar clinical efficacy in one indication, and the manufacturer submits a bit of extra data, then the biosimilar gets all the same indications on its package insert.
Happy to finally get a Road House reference on tl;dr! Image
Opinions vary on how big of a deal this is…
On the one hand, if a biosimilar has to go through the same clinical burden as the reference product, it won’t be cheaper to produce.
No drug company would make it, so the owners of the reference product can continue charging infinity-million dollars for their drug. There would be no competition in the market place to help drive down the price.
On the other hand, we can’t technically know if a biosimilar actually works for a disease it hasn’t been studied in. For all we know, we might be giving ineffective drugs to patients. To really grasp this point, read this article on the p-value that shows just how fickle the results of a study can be.
In my opinion, it’s “probably” fine for most biosimilars to extrapolate the indications. There are enough PK studies in the Totality of Evidence that we can reasonably assume they will work. And in the case of something like Retacrit, if a patient isn’t responding after a few doses, we can always try switching to the reference product.
But your patients have a right to know about this limitation, so keep it in mind.
We also get to see some really fun “legal technicalities” with evidence extrapolation.
Bevacizumab [Avastin] is used in the treatment of a variety of cancers. But it received approval as an Orphan Drug for the treatment of ovarian cancer.
Bevacizumab-awwb [Mvasi] is a biosimilar for Avastin. Thanks to indication extrapolation, it is approved for everything that Avastin is approved for…EXCEPT for ovarian cancer.
Since Avastin is an orphan drug for ovarian cancer, Mvasi can’t legally be promoted for this indication (yet).
The funny catch-22 is that the NCCN Guidelines for Ovarian Cancer are totally cool with using the biosimilar to Avastin. And since CMS and most payors look to NCCN to determine the appropriateness of therapy, you’re probably still going to see Mvasi used in ovarian cancer (much to the chagrin of Genentech).
Biosimilar Clinical Pearls
I’m not really sure what to call this section, so I’m just going to get right into a “stream of consciousness” of random thoughts.
With biosimilars, you’ll generally see the same side effects as the reference product. But just like with generic drugs, there may be some differences.
Some patients may not tolerate the biosimilar. Its manufacturing process may be completely different than the reference product, and a patient could have an allergy or intolerance to any part of the “soup” that makes up the biosimilar. It is totally prudent to switch the patient to the reference product if they don’t tolerate the biosimilar.
You can practically guarantee that the biosimilar has NOT been studied in the same combinations as the reference product.
For example, Herceptin (reference product) is frequently given with Perjeta. Can we give Kanjinti (biosimilar) along with Perjeta and expect the same benefit? Going further, if a patient tolerates their first dose of Herceptin, we speed up the infusion for subsequent doses. Can we do that with Kanjinti?
Finally, your sound clinical decision (and the wishes of your patient) may not matter all that much to the insurance company. Increasingly, payors may require a prescriber to use the biosimilar first. Only after a patient has failed (or didn’t tolerate) a biosimilar will the insurance company allow the use of the reference product.
In some cases, you may even see payors demand a biosimilar as a therapeutic interchange from a different drug. For example, I’ve heard stories of insurance companies demanding to use Retacrit in place of darbepoetin alfa [Aranesp]. Retacrit is NOT a biosimilar to Aranesp, they are entirely separate products.
Again, this isn’t a judgment call on what’s right or wrong — just highlighting what you’ll see out there. Quite honestly, we’re on the frontier with biosimilars. In general, I think that you’ll find most institutions using them exactly like the reference product. That includes administering them as a rapid infusion and using them in the same combinations with the same premeds as the reference product.
Is this the right thing to do?
¯\_(ツ)_/¯
I’m sure we’ll learn more as we keep using biosimilars and getting more data.
Additional Resources on Biosimilars
Good, bad, and ugly, biologics and biosimilars are here to stay. They’re an important (and growing) part of our health care system. As more reference products lose their patent, you’re going to see more biosimilars.
If you work in oncology, immunology, or rheumatology especially, you owe it to yourself to become very comfy with biosimilars.
I hope this post has given you a decent overview, but if you’re looking for more info, check out the following. Note that some of the references are from industry players such as Genentech…so there may be a financial bias lurking. But let’s not let that blind us to the fact that there is also really helpful info on these sites. And good information is good information:
Happy Biosimilaring!