The Complete (but Practical) Guide to Phenytoin Dosing
Editor's note: Stephanie Kujawski, PharmD, BCPS hardly needs any introduction to long-time readers of tl;dr pharmacy. She's written a super handy overview of pharmacokinetics. Then she wrote the best guide to vancomycin dosing I've ever seen. THEN she wrote an incredible guide to dosing aminoglycosides. After that, she helped us write Mastering the Match: How to Secure a Pharmacy Residency.
And now, she's back at it again. This time she's tackled phenytoin; a drug that's notoriously difficult to dose. Steph has a real talent at breaking down the dosing of these complicated drugs into easily digestible (yet useful) guides. And we really appreciate her taking the (massive) amounts of time required to share this info with you all. On top of all that, I'm consistently amazed by Steph's ability to work Star Wars references into everything she writes. Most impressive.
Anyway, watch your step...because Steph's about to drop some knowledge.
Would you like to print this article? Or save it for offline viewing? You can get it as an attractive and printer-friendly PDF right here.
Pharmacokinetics Dosing Wars: Episode the Last
Hello Pharmacy Phriends! Sorry for the hiatus from writing, but I promise I didn’t forget you. It’s just been a busy couple of months, what with packing my bags and moving halfway across the country. But now I’m back, and it’s for a goodie.
Today is the day we tackle phenytoin. I want you pumped and ready to take it down. Because it’s a beast even more beastly than the roguish wampa of vancomycin.
(I’m sorry, I just wanted to use the word rogue. Isn’t it quite a fantastic word??)
Anyways, I digress.
So let’s start with the basics. Phenytoin is, of course, one of the most classic anti-epileptic medications. It is used to both prevent and treat seizure disorders. Even though it is not quite as highly utilized in recent years due to the emergence of simpler, relatively happy-go-lucky drugs like levetiracetam and lacosamide, it is still very much on the bench and often called up to play.
Like many other anti-epileptic drugs (AEDs), we don’t reeeeally know exactly how phenytoin works… What we do know is it affects the transport of sodium ions across cell membranes.
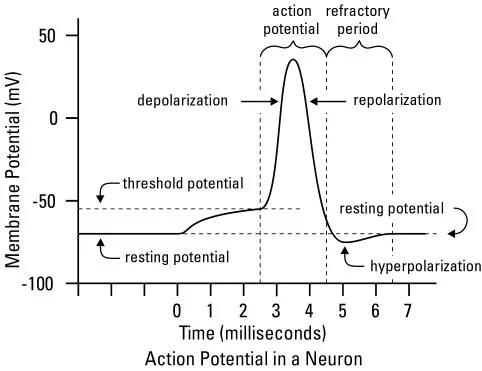
And if you go WAY back to biochemistry, remember sodium influx from the outside to the inside of the cell is what starts action potential propagation.
Here’s a look at the general action potential with electrolyte movement noted:
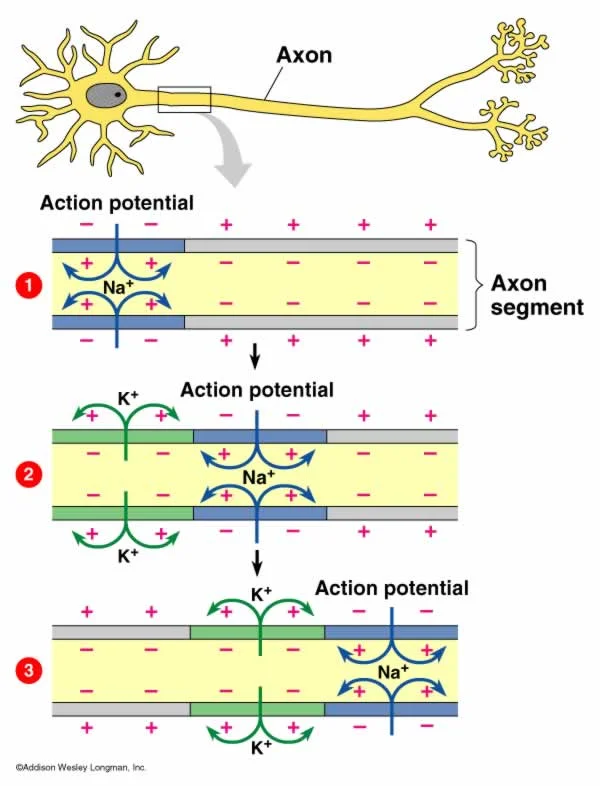
Now let’s take a look at how that relates to the depolarization and repolarization of a neuron:
And finally, let’s relate this to how action potentials move throughout a neuron:
So to summarize, by either slowing sodium influx into the cell or expediting efflux out of the cell (unknown how much of either), phenytoin slows action potentials. Which ultimately decreases the excitability of neurons and slows neuronal transmission. Which is what we want when treating seizures, right?
So what makes phenytoin seem like it’s a member of the Sith?
Kinetics. That’s what.
In every episode of Dosing Wars up till now, we’ve been discussing drugs that are predictable. We give a dose, we can generally estimate what’s going to happen to the serum concentration. We check a level, and if it’s not where we want it, we modify the dose accordingly.
Well isn’t that cute.
Now brace yourself for the Dark Side, peeps, because phenytoin doesn’t play nicely like that.
As opposed to linear kinetic drugs like vancomycin and aminoglycosides, phenytoin exhibits non-linear kinetics. Meaning a change in dose does NOT produce a proportional change in concentration. It’s also known as zero-order or saturable kinetics because metabolic mechanisms can literally become saturated. This causes a constant AMOUNT of drug to be eliminated over time rather than the constant PROPORTION of linear kinetics.
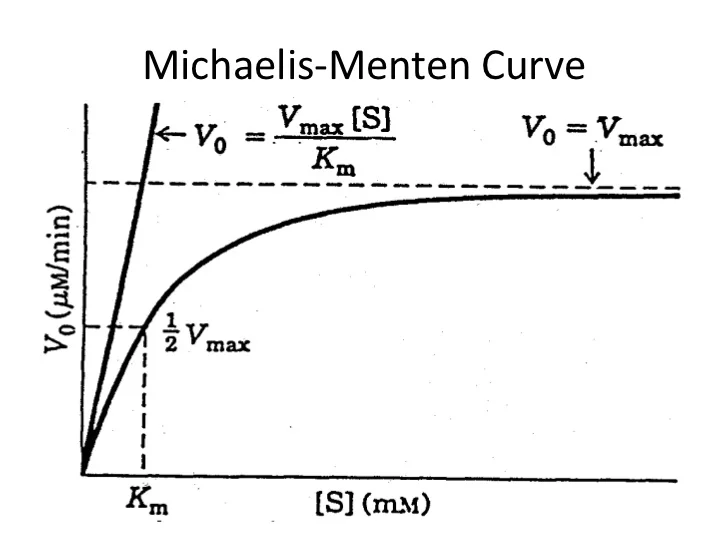
You may also have heard it called Michaelis-Mentin kinetics in memory of the 2 phenoms who studied these qualities of enzymes. In picture form:
Basically, ignore the equation, you’ll never need it. What you should take away from this is that while the concentration of unbound drug is low, the rate of hepatic metabolism is actually almost linear. You see that nice, almost straight, rising line that indicates proportional, first order elimination.
BUT, as you add more drug (aka move right along the x axis and increase intracellular drug concentration), the rate of hepatic metabolism slows, which is why the curve flattens.
The Km is the concentration at which half of the max elimination velocity (Vm) is reached. So above Km concentrations, you’re starting to approach max velocity of elimination and curve flattening, which is when it switches over to a constant amount being metabolized. You simply can’t get rid of drug any faster, the enzymes are saturated!
This whole process is also why the half-life of phenytoin changes with changing concentrations of drug. Increasing concentrations of drug means increasing t1/2, so it can range anywhere from 7-42 hours! So then when you figure about 5 half-lives to reach steady state…yeah, it can take a while...
Usually we say 5-7 days to reach steady state.
Regardless of the name and equations, the end result of nonlinear kinetics is this: far less predictable serum concentrations.
A brief note before we go any further…
When I first started writing this post, it quickly became apparent that this was going to be more difficult than the other posts in Dosing Wars. Much like its kinetics, phenytoin discussions just aren’t linear. There are too many pieces to keep track of.
So rather than have one long, linear post about how to dose phenytoin (like we did with vanc), we’re going to have to take this in pods. Below are the topics we’re about to tackle, and then we’ll put it all together with a dosing example.
Pod 1: Phenytoin Drug Formulations
Before we get too excited about jumping into dosing, there’s one piece I have to mention. We have to have a hot minute for fosphenytoin. Fosphenytoin is the water-soluble prodrug of phenytoin. It’s like the Anakin to Darth Vader.
Fosphenytoin is dosed in phenytoin equivalents (or PEs). All you have to remember about this is that fosphenytoin 1mg PE = phenytoin 1mg. So let's say you're dealing with status epilepticus, and your reference states that the dose of phenytoin for status epilepticus is phenytoin 20mg/kg. But maybe you only have fosphenytoin on hand (or you just want to use fosphenytoin because it's got a cool brand name, "Cerebyx").
Well, your dose is very easy: fosphenytoin 20mg PE/kg.
The manufacturers of fosphenytoin recognize this can be confusing. So they’ve made it easy for us. Every vial of fosphenytoin is labeled in PE, so you really don’t even really have to worry about it!
So we have 2 drugs that work the same way, are dosed the same, and are for the same purpose. You may be asking yourself why on earth do we have both? Wouldn’t it be easier to just worry about one?
Sure. But that was before drug shortages hit in earnest. Oh happy days of yore.
These days, fosphenytoin is a little like Luke in The Force Awakens. We know he’s out there…there have been sightings…but we’re not 100% certain he’s for real back. So for now we have to know about both drugs.
Anyways. Back to fosphenytoin being the Anakin to phenytoin’s Darth Vader. Fosphenytoin fits this analogy in several ways. For starters, it's a pro-drug (or a precursor) for phenytoin, in the same way that Anakin is a precursor to Darth Vader. And secondly, fosphenytoin, like Anakin, is just plain nicer than its counterpart (at least in terms of administration).
You can see from this table that fosphenytoin offers increased flexibility in route and rate of administration, as well as better compatibility with fluids. You can imagine if someone is in the middle of seizing, we’d want to get the drug into them ASAP, which can be a little slower and harder with plain phenytoin. For these reasons, we love fosphenytoin and are super hopeful that it’s back for real this time.
This looks totally normal, right?
Regardless of whether you use phenytoin or fosphenytoin, we need to monitor for adverse effects, including cardiac toxicities like hypotension and arrhythmias. Infusion can also lead to “purple glove syndrome”, which may or may not be due to extravasation.
I guess while we’ve wandered into adverse effects, we might as well do it right.
Here are some more adverse effects to be aware of when maintaining people on phenytoin:
The gingival hyperplasia struggle is real.
Phenytoin Dose-Independent Adverse Effects
Hypertrichosis/hirsutism
Gingival hyperplasia
Coarsening of facial features
Hyperglycemia
Blood dyscrasias
Leukopenia, thrombocytopenia, agranulocytosis, pancytopenia +/- bone marrow suppression
Lymphadenopathy
Decreased bone mineral density (vitamin D deficiency)
Dermatologic reactions, including Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN)
Hepatotoxicity
Peripheral neuropathy
Phenytoin Dose-Dependent Adverse Effects (aka indications of phenytoin toxicity)
Nausea/vomiting (early)
Nystagmus
Ataxia
CNS depression (including coma and possible respiratory failure)
Pod 2: Phenytoin Protein Binding and Volume of Distribution (Vd)
One of the reasons phenytoin is so difficult to predict is because it is highly protein bound. Up to 90-95% of the drug can be attached to proteins like albumin. Which means there’s usually about 10% free (log that number away in your brain for later).
Think of it like this…phenytoin bound to protein is phenytoin not actively preventing seizures. Only the free phenytoin is actually fighting the Dark Side of seizures. But like Luke Skywalker, bound phenytoin is just waiting in the wings for the right time to show itself against the enemy, and so it still has to be accounted for! Which we do with total levels. More to come.
This high degree of protein binding is at least part of what contributes to phenytoin’s relatively large volume of distribution. In general, the population kinetics estimate for phenytoin in adults is a Vd of 0.7 L/kg.
So, assuming an average 75 kg person, the Vd of the drug by calculation is going to be 52 L. The average total body fluid in a person is juuuust abouuut 45 L. So the drug HAS to be going somewhere!
And it is: to the protein. So, remember that phenytoin has a decently large volume of distribution, due in large part to the protein binding.
Of course, the seizure-fighting troops never stay in one place. Phenytoin is constantly finding equilibrium binding and unbinding to proteins. And disease states that alter the amount of protein in the serum can therefore alter the amount of phenytoin that's free and ready to fight seizures.
To name just a few disease states that can result in decreased levels of albumin and an altered Vd:
Malnourishment
Renal failure/uremia
Burns
Cirrhosis
Pregnancy
All of these can result in more free and active phenytoin.
Pod 3: Phenytoin Dosing and Dosing Weight
In general, phenytoin is dosed based on ideal (aka lean) body weight. I’m sorry, I don’t have a good explanation or rationale for why that is (given its extensive Vd), but we just have to go with it.
So, for most patients, you would use your normal IBW equations to find the dosing weight for loading and maintenance doses.
The exception to this is if your patient is obese, aka their total body weight is at least 25% over their ideal. (Some institutions consider it 20% over, others use 30% as their cutoff…whatever, close enough). In these obese patients, we would use an adjusted body weight for both loading and maintenance doses.
To make it a bit more tricky, there are 2 different adjusted body weights for phenytoin. For an initial, weight-based loading dose of phenytoin, the adjusted body weight is calculated using a larger correction coefficient (to account for "filling the empty tank" per se), so:
Initial Load AdjBW = 1.33*(TBW – IBW) + IBW
For any subsequent mini loading doses given for subtherapeutic levels (aka NOT a completely empty tank) or for maintenance dosing, a regular adjusted body weight correction coefficient is utilized:
Subsequent Load AdjBW = 0.4*(TBW – IBW) + IBW
Confusing, I know. But just remember these two points:
Non-obese people are dosed on ideal body weight, and obese people are dosed using adjusted body weight.
There are 2 adjusted body weight equations depending on whether you’re starting from scratch or not.
Initial loading doses of phenytoin are usually 20 mg/kg of the appropriate dosing weight as above. Mini loads for subtherapeutic subsequent levels are typically 10 mg/kg (quick disclaimer: you may see anywhere from 5 - 15 mg/kg given as a mini load. I'll just use 10 mg/kg moving forward to make things simple). A general scheme for maintenance dosing is 5-7 mg/kg/day, although this may be empirically lowered to less per day if a patient is severely hypoalbuminemic.
So again, to make it purdy:
Initial loading dose: 20 mg/kg
Mini-loading dose (for subtherapeutic levels): 10 mg/kg
Maintenance dose: 5 - 7 mg/kg/day (but adjust for severe hypoalbuminemia)
One more important note about dosing. If utilizing PO dosing, anything above 350mg should be split into multiple smaller doses to aid with absorption.
This goes for both maintenance and any mini loading PO doses. So you can imagine that, for PO loads, you may have several small doses given every 2 hours to make a cumulative dose.
Pod 4: Drug Interactions, Vd, and Drug In
Along the train of thought about free versus bound phenytoin and volume of distribution, we the pharmacists have to First Think Drugs (#FTD!).
Aka, we have to consider drugs that might affect phenytoin’s distribution. Some drugs compete with phenytoin for its protein hiding spots, and there are many that displace phenytoin from albumin (most notably, valproic acid...but basically anything that's greater than 80 or 90% protein bound). So we have to be cognizant of these drug interactions that can affect how much phenytoin is free and fighting seizures versus how much is bound to protein and waiting in the wings.
Also, be aware of drug/nutrient interactions that can inhibit absorption of PO phenytoin doses…especially tube feeds! In particular, phenytoin seems to like binding to proteins and calcium. It can even bind to the tube itself! So separation and flushing are imperative when giving PO phenytoin to patients receiving this type of nutrition.
Pod 5: Drug Interactions, Metabolism, and Drug Out
Drug interactions also play a role in the metabolism and drug out considerations for phenytoin. If you remember nothing else from this post, take this away:
CHECK FOR DRUG INTERACTIONS!
Phenytoin is metabolized by several CYP enzymes (mainly 2C19, and 2C9, but a little of 3A4 too), and so there are multiple medications that can affect its metabolism.
So regardless of mechanism of altered phenytoin concentrations (aka changes in distribution versus metabolism), see below for a sampling of medications that can affect phenytoin serum concentrations:
FYI, on the other hand, phenytoin is a potent inducer of multiple CYP enzymes as well as Pgp and UGT1A1, and so it can affect other medications in a highly significant manner. (Did someone say WARFARIN!?!).
Although the focus for this post is on phenytoin dosing, it’s hard to mention drug interactions of phenytoin and ONLY discuss the ones that affect phenytoin. We have to at least mention that phenytoin affects many other drugs as well!
So the road goes both ways here. Check for drugs that can affect phenytoin AND for drugs that phenytoin can affect.
POD 6: Phenytoin Clearance
With all this talk of hepatic metabolism, it’s easy to forget about the physical removal of the drug from the body. Plus there’s not that much exciting here, but for completeness, we’ll mention it.
Phenytoin may be oxidized by hepatic CYP enzymes, but it is excreted by the kidneys following glucuronidation. Less than 5% is excreted as unchanged drug, so that gives you an idea of how much work the body does on this med! Pharmacokinetics in action here, y’all.
THE BIG POD: Phenytoin Levels
So now that we have all those pods out of the way...
How the heck are you, the pharmacist, supposed to monitor this drug if there’s all this business about free and bound phenytoin…AND account for drug interactions?!?
Luckily, this is a drug we can monitor via serum levels. Hallelujah! Otherwise, we’d be screwed.
Because of its protein binding, there are two things we need to keep track of for phenytoin:
How much drug is free to fight seizures
The total amount of drug in the body
We do this by checking both free (aka unbound) and total (aka unbound AND bound) levels.
In a patient with normal albumin levels, goal total phenytoin levels are 10-20 mcg/mL. This is based on the fact that we want our free (therapeutically active) levels to be between 1-2 mcg/mL, and normally about 10% of the drug is free and unbound. (Remember way back when I said to log that number away??). So 1-2 mcg/mL is 10% of 10-20 mcg/mL.
Goal Total Phenytoin Level: 10 - 20 mcg/ml (assuming normal albumin)
Goal Free Phenytoin Level: 1 - 2 mcg/ml (for both normal and abnormal albumin)
Now if a patient does NOT have normal albumin levels and/or has drug interactions that can affect protein binding of phenytoin, then your goal total levels will change.
You will ALWAYS want your free levels to be 1-2 mcg/mL because that’s what we require to fight seizures, but if your actual free percentage (or free fraction as we like to say in practice) for a patient is not the standard 10% (or 0.1 in fraction terms) due to the above factors, then your goal total levels will change. This new goal total range can easily be back calculated, which we’ll discuss.
In terms of timing of levels, it kind of depends on the situation. Remember that steady state takes 5 - 7 days to reach. (Oh let’s just say a week for simplicity’s sake).
So you’re not going to get steady state levels in a patient who’s emergently seizing and you just loaded with phenytoin for the first time. But you do at least want to know if you’re touching your initial goal therapeutic range of totals 10-20 mcg/mL or whether you need to give more drug in the emergent period.
So for emergent situations, you can check a total phenytoin level at least 2 hours after completion of an IV load (you have to allow time for distribution to proteins).
If you happened to do a PO load for whatever reason, you should wait at least 24 hours to check a total level.
For routine monitoring of maintenance doses, it’s ideal to check both free and total levels. This should be done as a trough (or at least 2 hours after the last dose) to ensure maximal distribution time. The exception to this is if a patient is taking the extended release formulation, in which case timing of levels is less crucial.
Doing both free and total levels allows you to calculate a patient-specific free fraction (ff) to see how close you are to the ideal 10%:
ff = (free phenytoin level/total phenytoin level)*100%
Knowing your patient’s free fraction also allows you to calculate their goal total levels. The below strategy back calculates total levels by rearranging the above ff equation and inputting free levels of 1 and 2 mcg/mL, since that is the range of free levels we know to be therapeutic. Check it out:
Goal total level range = 1/ff to 2/ff, where the ff is in decimal (not percentage) form
Thereafter, as long as your patient’s albumin and binding properties stay fairly stable, you really only have to check total phenytoin levels. (Free levels cost mucho $$!).
Of course, the caveat is if your patient goes into renal failure…or has a new interacting medication added to their regimen…anything that can change the ff. Then you’ll have to re-establish that free fraction again.
A quick note about levels…
Some institutions and practitioners will utilize correction equations (like the traditional Winter-Tozer and its iterations) to interpret whether measured total phenytoin levels for their patients actually fall within the therapeutic range. These equations are used in place of obtaining a (pricey) free level and calculating a patient specific free fraction.
While they supposedly take into account hypoalbuminemia and uremia, their accuracy has been shown to be limited in studies that compared equation-calculated versus measured free levels, especially in hypoalbuminemic patients. Not to mention the variability that comes from genetics (CYP polymorphisms) and drug interactions.
So, basically, if possible, actually measure your patients’ free levels to establish a free fraction!
Putting it all together...
Phenytoin Case Study: Save the Princess!
LO is a 55 YOF (5’7”, 115 kg) admitted to the hospital for new onset seizure disorder. She has stopped seizing with lorazepam 2mg IV x2. Her albumin is 1.8 g/dL, and her SCr is 0.8 mg/dL. The neurologist would like to begin phenytoin. What IV loading dose will you enter? What IV maintenance dose will you start and when?
Let's approach this in a stepwise manner...
Is she obese?
LBW = 45.5 + 2.3 (7) = 61.6 kg
TBW = 115 kg
115/61.6 kg = 186% of LBW
(Yes, she's obese).
Calculate adjusted body weight for the initial load (AdBW(L))
AdBW(L) = LBW + 1.33*(TBW – LBW) = 61.6 + 1.33*(115 – 61.6) = 132.6 kg
Calculate initial loading dose
LD = 15 – 20 mg/kg*(AdBW(L)) = 15 – 20*(132.6 kg) = 1989 – 2652 mg
Order phenytoin 2000, 2250, or 2500 mg IV x1
Duration of infusion?
Max infusion rate = 50 mg/min
E.g., Infuse over at least 45 min (for the 2250 mg dose)
Since she is obese, calculate adjusted body weight for maintenance dose [and any subsequent loads (AdBW(M))]
AdBW(M) = LBW + 0.4*(TBW-LBW) = 61.6 + 0.4*(115-61.6) = 83 kg
Calculate maintenance dose (usually 5-7 mg/kg/day). Since she is so hypoalbuminemic, however, we’ll empirically utilize a lower dose of 4 mg/kg/day to account for a likely increased ff.
4 mg/kg/day*83 kg = 332 mg/day ~ 300-350 mg/day
Order phenytoin 100mg IV TID
When should the maintenance dose begin?
18-24 hours after completion of the loading dose
What levels should be ordered and for when?
Check free and total levels at least 2 hours after the end of the IV load, but practically speaking, it is often done the next day. These levels, of course, will not be at steady state, but they will tell you if you’re protecting against seizures at that time.
On day #2, the total and free levels are reported as 2.9 and 0.5 mcg/mL, respectively. No further seizures have occurred.
What is L.O.’s free fraction?
0.5/2.9*100% = 17.2%
What is L.O.’s goal total phenytoin concentration range?
Range = 1/ff to 2/ff = 1/0.172 to 2/0.172 = 5.8 to 11.6 mcg/mL
Is L.O. in therapeutic range?
No, free concentration is not within 1-2 mcg/mL, and total concentration is only 2.9 mcg/mL. She is not protected against seizures.
Next steps since she is not protected?
Give L.O. a mini phenytoin loading dose of 10mg/kg based on AdBW of 83kg
Leave maintenance the same as it is only day #2 of therapy (not at steady state)
On day #5, the total level is reported as 9 mcg/mL. Her albumin is stable. No further seizures have occurred.
What is L.O.’s free phenytoin concentration?
Free = Total * ff = 9 * 0.172 = 1.5 mcg/mL
Is L.O. in therapeutic range?
Yes, free level is within range of 1-2 mcg/mL, and total is within her specific goal range of 5.8-11.6 mcg/mL.
Next steps?
Leave dose as is and recheck total level in another 7 days.
WHAT IF…
On day #5, the total level is reported as 4.9 mcg/mL. No further seizures have occurred.
What is L.O.’s free phenytoin concentration?
Free = Total * ff = 4.9 * 0.172 = 0.84 mcg/mL
Is L.O. in therapeutic range?
No, free level is below therapeutic range of 1-2 mcg/mL, and total is below her specific goal range of 5.8-11.6 mcg/mL
Next steps?
Give mini loading dose of 10 mg/kg either IV or PO to ensure adequate seizure protection
Go ahead and increase maintenance dose by 50 mg/day (since approaching steady state by day 5). Maintenance doses are not usually increased by more than 50 mg/day at a time given nonlinear kinetics.
Recheck total levels the next day
Rinse and repeat!
Remember, you can give mini loads of 10 mg/kg IV or PO when needed for subtherapeutic levels to ensure adequate protection at a particular moment in time. However, avoid increasing maintenance doses too quickly in succession from daily levels (remember nonlinear kinetics)!
Eventually that will catch up, and enzyme saturation will occur. And then you’ll have supratherapeutic levels...and potentially a somnolent princess with twitchy eyes! So not a pretty picture.
OK, so that’s the gist of phenytoin!
I know it’s a ton of info, but read and re-read at will. If you take absolutely nothing else away from this post, remember these main points:
Phenytoin is nonlinear – small dose changes go a long way!
Consider diseases and drugs that can alter protein binding and ALWAYS check drug interactions
Establish a patient-specific free fraction to aid in assessment of total levels
So, who wants to recommend levetiracetam now?