The ABCs of RLS: Restless Legs Syndrome
Steph’s Note: This week, we return with a clinical disease state review. It’s elusive, it’s multi-factorial, and the pharmacotherapy honestly just isn’t all that successful just yet. But even if we’re still in the "“if at first you don’t succeed, try, try again” phase for this disease state, we pharmacists should certainly be familiar with the attempts! So here to teach us is Tanin Motamedi.
Tanin is a fourth year pharmacy student from Howard University College of Pharmacy. She has a BS in Neuroscience from George Mason University and is interested in the complex neurochemical interactions within the body and their prominent implication in pharmacy. After graduation, she hopes to be in a regulatory role with a focus in neuropharmacology.
(Image)
What is Restless Legs Syndrome?
Restless Leg Syndrome (RLS), also known as Willis-Ekborn disease, is a neurological condition that affects about 12% of the US population. The two categories of RLS are primary and secondary. Primary RLS occurs in otherwise healthy adults, while secondary can stem from a list of conditions as lengthy as a local CVS receipt for a single pack of winterfresh gum.
Symptoms of RLS include discomfort resulting from a creeping, crawling, pulling, and stretching sensation. This is known as paresthesia, which can be experienced not only in an individual’s legs but also (unlike the name “RLS” suggests) the arms and other areas of the body. These symptoms can be present during the day but are known to peak at night, eliciting jerk-like movements known as periodic limb movements (PLMs) — arguably the most important diagnostic criteria for RLS.
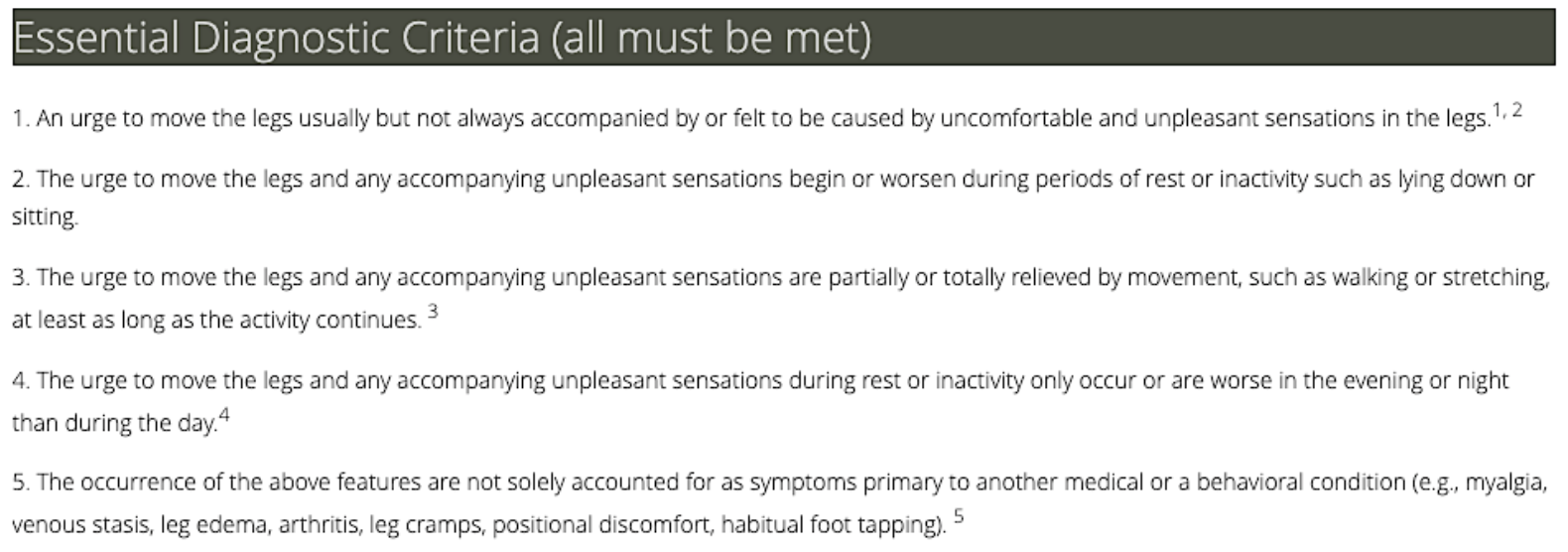
The International RLS Study Group, dedicated to advancing basic and clinical knowledge on the condition, identified the five essential criteria for RLS diagnosis:
(Image)
This same organization has also developed a quantitative severity scale (IRLS), considered to be the gold standard, which asks patients a series of 10 questions to rate symptoms from 0 (having no symptoms) to 4 (having very severe symptoms). The Johns Hopkins Severity Scale (JHSS) is one commonly-used alternative, as are various questionnaires that assess general quality of life.
Pathophysiology of RLS
The medical sciences, as anyone in the community can attest to, possess an unusual commitment to non-committal verbiage. RLS is no exception, with numerous studies aimed at decoding its pathophysiology, only to end up using phrases like “this may suggest,” “one possible interpretation,” and “inconsistent findings.” So, here’s a list of things we do know about the pathophysiology of this condition: dopamine, iron, and genetics.
The Role of Dopamine in RLS
One of the diagnostic procedures to confirm RLS is known as the levodopa test, in which a single 100 mg levodopa tablet is given to the patient. If symptoms are reduced by at least 50%, then the patient is determined to have RLS. Due to this responsiveness, the dopaminergic pathway has remained the principal focus of RLS studies and is considered to play a key role in its pathology.
Cross section of the brain in case it’s been a while since you’ve visited the amygdala… (Image)
There are five variations of dopamine receptors (D1-D5) that are primarily expressed in the central nervous system, while others reside in the periphery, such as the vasculature and kidneys. These receptors act through a push-pull mechanism. This means that the stimulation of some receptors, notably D1 and D5, increases excitability, while the stimulation of other receptors, D2 to D4, reduces excitability. The excitatory receptors D1 and D5 exist in high density in the striatum and nucleus accumbens, regions of the brain that heavily regulate emotional and cognitive processing as well as voluntary movements. These receptors are also seen in the substantia nigra, a critical region for dopamine development.
Expectedly, the D1 and D5 receptors are involved in memory and attention regulation, impulse control, decision making, locomotion, and to a lesser degree, regulation of certain renal functions (which we will willfully disregard for our purposes today). The inhibitory receptors D2, D3, and D4 are more or less concentrated in the same areas in addition to the hippocampus— a region implicated in learning and memory—and the amygdala—the center for the old “fight-or-flight” adage.
Some study results have shown reduced, increased, and/or unchanged receptor binding at either, or both, the presynaptic and postsynaptic sites.
Clear as mud, right?
Quick review of the 4 major pathways for dopamine in the brain. For the purposes of this RLS post, we’re focused on the nigrostriatal pathway involved in motor functions. (But it never hurts to take an extra moment to consider how the other pathways may play a role with pharmacology - especially the antipsychotics!)
What the studies consistently agree on, however, is an element of receptor dysfunction originating from the A11 dopaminergic cells, which (here it comes) may suggest a potential anatomical site for the dysfunction. These cells are located in the midbrain adjacent to the hypothalamus, and they are the only subtype of this cell group with long axonal projections that extend to the spinal cord before arriving in motoneuronal sites. This characteristic may explain the spasmodic movements.
Considered a major source of dopamine in the spinal cord, A11 cell lesions, which have been tested in rats, have been shown to result in increased RLS-like movements, including PLMs. Previous studies have also suggested that the proximity of this system to the circadian control centers of the hypothalamus could be a cause of sleep disruptions in RLS patients.
Iron and RLS
(Image)
The next area of relative certainty in RLS patients is iron deficiency. Iron is a cofactor for the enzyme tyrosine hydroxylase, which in the flow diagram to the right, is responsible for the rate-limiting step in the conversion of the amino acid tyrosine to levodopa. Levodopa then goes on to be converted into dopamine (which in turn is converted into other catecholamines!). Therefore, iron deficiency directly affects the availability of dopamine (as well as other catecholamine neurotransmitters).
MRI studies in RLS patients were able to confirm the following:
Low iron concentrations in the substantia nigra (remember, this is a major site for dopamine production)
Decreased ferritin concentration in the cerebral spinal fluid
Decreased transferrin receptor expression in the brain (the receptor responsible for the import of iron into cells)
Oral or intravenous iron treatment has been shown to significantly decrease symptom severity in iron-deficient RLS patients.
The Genetics of RLS
From a genetic standpoint, the International RLS Study Group lists the presence of positive family history as a supportive diagnostic criteria. About 40% of RLS cases have a positive family history of dominant inheritance, with studies able to confirm eight different loci in five chromosomal positions associated with RLS.
Although genetics remains an under-studied component of the disease, data does show that it plays a fundamental role in disease pathology.
Alright, now that we’ve established the roles of dopamine, iron, and genetics, what chance do we have of combating RLS in these 3 arenas?
Management of RLS
Due to the ambiguity of RLS’s pathophysiology and diagnosis, none of its currently approved treatments are fully effective, especially especially when considering long-term management. Thus, those afflicted often try a combination of pharmacological and non-pharmacological options to keep symptoms at bay.
Pharmacotherapy for RLS Treatment
Quinine, an anti-malarial drug, was once used for decades to treat idiopathic muscular cramps and seemed quite effective in reducing RLS symptoms—until it wasn’t. In 2006, the FDA issued a warning about quinine’s off-label use for RLS, citing “665 reports of adverse events with serious outcomes.” Those “serious outcomes” were death! Studies conducted since then have shown that the drug’s long-term use is associated with a three-fold increase in mortality, primarily via sudden cardiac arrest. Even quinine’s short-term use has been shown to cause serious harm, with effects such as thrombocytopenia, hypoglycemia, and cardiac arrhythmias.
Fun fact: tonic water (aka the tonic in a gin and tonic) also contains quinine! In one 2017 analysis of over 125,000 individuals, there was a 25% increased risk of all-cause mortality in people who took just 200-299 mg quinine/day. A liter of tonic water has about 100mg of quinine, so it’s certainly less concentrated than taking a pill or two. BUT depending on how many G&Ts a person is having in a day…it could be clinically significant!
So not exactly a case of benefit outweighing risk with quinine. Just don’t do it.
After the quinine debacle, dopamine agonists became, for many years, the first line of treatment. Drugs such as ropinirole (Requip), pramipexole (Mirapex), and rotigotine (Neupro)—a drug approved in April 2012 that comes in transdermal patches—had previously been approved for Parkinson’s disease but are now also FDA-approved for RLS. Each drug’s initiating dose in an RLS patient is significantly lower than dosage amounts allotted for Parkinson’s patients. Additionally, these drugs can be slowly titrated every few days until working up to a maximum dose.
These agents, however, traditionally perform well only in short-term use in patients without preexisting heart conditions. Oh, and mental health concerns, which, in a post-pandemic landscape, is more of a rarity than ever. Due to the push-pull mechanism of dopamine receptors, the long-term use of these agents is highly associated with symptom augmentation, which refers to the paradoxical worsening of symptoms over time both in emergence and severity.
Given these treatments act on an intricate (and not yet fully understood) neurological pathway, they come equipped with a set of adverse reactions that range from compulsive behavior (e.g., gambling, excessive shopping, and hypersexuality) to hallucinations, sudden periods of extreme fatigue, and exacerbation of other preexisting mental conditions.
Dopamine agonists are also known to elevate blood pressure and elicit heart rate irregularities. Therefore, it’s critical for patients to gradually titrate and taper to avoid an onset of withdrawal symptoms.
Levodopa/carbidopa (Sinemet), though not technically a dopamine agonist, works in a similar manner in that its goal is to increase dopamine effects. How it does this is pretty darn pharmacologically elegant! In a perfect world, we could just administer oral dopamine to patients who need a dopaminergic boost for their RLS symptoms. But noooo the body has to be more complicated that this (of course).
The catch? Peripheral dopamine can’t cross the blood brain barrier to get to the CNS regions necessary to impact locomotor functions. Fooey.
Frodo:levodopa::Aragorn:carbidopa. We won’t go quite so far as to compare one’s CNS to Mount Doom because that seems destructive…(Image)
But on the other hand, dopamine’s precursor, levodopa, is crafty and can cross the blood brain barrier into the CNS from the periphery! Once in the CNS, it can then be converted to the shining beacon of RLS hope: dopamine. Unfortunately, Achilles heel warning, levodopa is also rapidly converted into dopamine in the peripheral tissues - BEFORE it can reach the CNS. So how do we ensure this precious levodopa molecule can actually reach its CNS destination without being converted? We give it a bodyguard: carbidopa.
Carbidopa is a dopa decarboxylase inhibitor, meaning it inhibits the enzyme responsible for converting levodopa into dopamine. So much like Aragorn took on the task of ensuring Frodo made it to Mount Doom, carbidopa ensures levodopa makes it intact from the periphery to the CNS, where it then completes its dopaminergic mission.
An elegant pharmaceutical tactic, eh?!?!
But this dopaminergic mission also means levodopa/carbidopa is associated with some of the same concerns as the true dopamine agonists. It is recommended to start this particular treatment with the lowest possible dose (100/25 mg), which can then be titrated if necessary. Levodopa is not known to induce as many behavioral concerns, but its dopaminergic activity does cause symptom augmentation.
This treatment requires increasingly higher doses over time to control symptoms, which can contribute to surges in erratic adverse events - so it’s fallen out of favor due to its unpredictability. One way to remedy adverse reactions is to gradually taper down dosage and switch to alternative agents such as gabapentin.
That brings us to the next class of agents, the GABA analogues: gabapentin and pregabalin. These selectively bind to calcium channels and allow charged calcium ions to move into nerve cells, an important stabilizing factor for neuronal electrical activity. For this reason, these agents are often used to treat a variety of neuron-related conditions, such as neuropathic pain, insomnia, and depression. Gabapentin and pregabalin have also shown greater efficacy than dopamine agents, while yielding significantly more tolerable side effects.
The prodrug gabapentin enacapril, under the brand name Horizant, was approved for RLS in June 2011 and comes with specific, daily dosing instructions of 600 mg taken once daily at 5 p.m. It should be avoided in older adults with a history of falls, however, as it may cause syncope and impaired psychomotor function. The drug is also associated with dizziness, somnolence, headache, and suicidal ideation that generally occur in the first week of therapy.
Pregabalin, meanwhile, has a recommended dose starting at 50 mg that can be titrated up to 300 mg. It is supposed to be taken 1-2 hours before bedtime to ensure it has adequately kicked in by the time of normal symptom onset. It, too, is generally well-tolerated but may cause some dizziness and somnolence.
The struggle with daytime sleepiness is real. Ask this baby. (Image)
Sedative hypnotics are the next class of most commonly-used agents. These benzodiazepines and benzodiazepine receptor agonists (BRA) impose their sedating effects by facilitating GABAergic transmission. These agents are more effective for patients with mild symptoms related to sleep disturbances. Although there is no evidence endorsing its clinical superiority, clonazepam is considered the treatment of choice and is to be taken orally in 0.5-2 mg doses prior to bedtime. There remains concern, however, with carry-over sedation due to the drug’s long half-life (not to mention hello! Beer’s criteria in the elderly), in which case, alternative agents within the BRA class with shorter half-lives, such as zolpidem and zaleplon, can be considered. Those also come with their own risks, however, such as sleep walking and sleep eating disorders.
Low potency opioids such as codeine, pentazocine, and meperidine, as well as medium potency opioids like hydrocodone and tramadol, have also been used to treat RLS patients who experience mild-to-moderate pain or discomfort on a daily basis. One study showed that an estimated 85% to 90% of patients using opioids remained on the drug years after initiation, compared to 20% of patients who used dopamine therapy. Tolerance and dependence seems to be less of a concern with opioids when used for RLS as it is not given for chronic pain but for abnormal and uncomfortable sensations. Therefore, patients are less likely to develop dependence based on its analgesic effects, but the risk of long-term use still cannot be ruled out.
As previously discussed, iron deficiency is a possible cause of RLS that can further contribute to dopamine dysfunction. Normal iron levels for men and women span a broad spectrum, so in this case, “low iron” is defined as a ferritin less than 75 mcg/L. Once iron deficiency is identified in a patient experiencing RLS symptoms, iron therapy often helps reduce severity and occurrence. The recommended oral dosage of this treatment is the equivalent of 65-85 mg of elemental iron per day, which oftentimes can be achieved as 325 mg ferrous sulfate once a day.
Oral iron is to be taken on an empty stomach (at least an hour before or two hours after eating) and should be supplemented with 100-200 mg of vitamin C for increased intestinal solubility. It is also recommended to drink plenty of fluids and increase fiber intake to avoid iron-induced constipation. Iron levels are to be checked every 3 months until serum ferritin levels reach 100 mcg/L. Intravenous iron is considered an acceptable alternative in the most severe cases.
Non-Pharmacologic Management of RLS
Evidence-based practice for non-pharmacological approaches is not well-established, but several isolated studies have shown remedial efficacy for RLS patients sans an exhaustive list of adverse events. While avoiding aggregating factors like alcohol, caffeine, and nicotine, the application of heat compressions, warm baths, and massage therapy have all been shown to alleviate some discomforts and associated sensations. Multiple controlled studies also suggest that aerobic exercise and lower body resistance training significantly reduces RLS severity, while more rigorous physical exertion (e.g., hot yoga, long-distance running, etc.) worsen symptoms.
This person… fighting RLS 0 miles at a time. (Image)
Several other non-conventional methods remain worth exploring. For instance, one of these is cognitive behavioral therapy (CBT) in RLS patients, which consists of sleep education, sleep hygiene, and relaxation techniques. In one study, 25 participants underwent CBT in a group setting for eight 90-minute sessions. Both the RLS-related quality of life and mental health status of the subjects improved significantly. Improvements persisted at a 3-month follow-up.
Another controlled study featured 25 patients who completed four 60-minute individual training sessions on general sleep education, stimulus control and sleep compression, and cognitive and relaxation therapy. Patients at the end of the study displayed significant improvements in severity of insomnia symptoms, subjective sleep efficiency, total sleep time, latency to sleep onset, wake after sleep onset, objective latency to sleep onset, and anxiety when compared to the control group.
The TMS procedure (non-invasive). (Image)
One compelling approach that yields similarly promising outcomes is transcranial magnetic stimulation (TMS), a non-invasive, painless procedure that uses magnetic pulses to stimulate neurons in specific areas of the brain via an electromagnetic coil against the scalp. This method has previously been employed as a last-resort treatment for depression, PTSD, OCD, or anxiety. Studies in which patients were treated over multiple sessions using different pulse frequencies directed at the motor areas of the brain showed at least a 50% decrease of symptoms, which continued to improve in the following months.
You may have heard of acupuncture in a trendy Real Housewives of Beverly Hills way as a method of alleviating extreme duress due to a minor inconvenience, but the technique has long been employed in traditional Chinese medicine as a method of treating pain, managing stress, and improving overall wellness. The procedure, which entails inserting extremely thin needles through the skin at specific points aptly called acupoints, has previously been studied in the context of RLS symptom management, but each study yielded inconclusive results given variations of treatment and fluctuating individual response.
(Steph was going to insert an acupuncture image here, but after googling acupuncture, she decided people didn’t really need to pass out over an RLS post.)
One such unique (and perhaps a smidge sketchy) study was conducted on two RLS patients who received a combination of acupuncture and a point injection of pentazocine, an opiate analgesic traditionally taken orally to treat moderate to severe pain. In this particular study, 0.25 mL of normal saline supplemented by 0.5-1 mg of pentazocine was acuinjected at four specific acupoints in both legs via a ¾-inch needle. In the first patient, PLMs decreased and sleep efficiency increased. Similarly, the second patient experienced near-complete suppression of PLMs and the patient reported “remarkably restorative sleep” the next morning.
The tl;dr of RLS
At its core, RLS remains elusive to scientific understanding. It can be viewed as a neurobiological disease based on current findings of nerve dysfunction and genetic inheritance, but palliative pharmacotherapy is far from sufficient and often leads to a more complicated disease state due to symptom augmentation. Regardless of severity, a specific and individually-tailored combination of pharmacotherapy and non-pharmacological options would be the most beneficial approach to treat those suffering from RLS.