Pharmacotherapy of Mucositis
Steph’s Note: Whether you’re an oncology pharmacist or just a general practitioner, everyone needs to know at least a little bit about this incredibly common (and very impactful) adverse effect of chemotherapy. So to get y’all up to speed, Jenny Nguyen is here to share her expertise!
Jenny Nguyen, PharmD, born and raised in Minnesota, received her Doctor of Pharmacy degree from the University of Minnesota College of Pharmacy. Dr. Nguyen completed her PGY-1 training at M Health Fairview- Woodwinds hospital and is currently finishing her PGY-2 Hematology/Oncology residency at the University of Minnesota Medical Center/ Masonic Cancer Clinic. In her free time she enjoys traveling, hiking, hitting up Taco Bell, & reading Amazon reviews (and buying things she doesn't need). Post-residency, she is excited to take a month-long nap before she continues her oncology career at Mayo Clinic.
What is Mucositis?
Mucositis is considered a hallmark - bread and butter - toxicity of chemotherapy. It’s the side effect that you may not initially think about, until it last-minute, ninja-style sneaks up on you. Kind of like that CV you’ve been meaning to update.
If you are looking for a sign, this is it! Go update that CV! Or hang here with us for a few first and then attack your CV.
Anyways, back to what I was saying… Mucositis, if left ignored, can have some serious consequences for our patients with cancer, including decreased oral/nutritional intake, uncontrolled pain, treatment delays, infection risk, and in some cases prolonged hospital stays.
So what IS mucositis anyways?
By definition, muco= mucor, and itis= inflammation. So it is the inflammation of the mucous membranes. “Mucous? Like the stuff that comes out of your nose?”
No, no it’s snot. (Harrrr.)
Mucous membranes line various cavities of the body and internal organs, such as the oral cavity, esophagus, and gastrointestinal (GI) tract. They consist of one or more layers of epithelial cells, which are the first cell types that come into contact with external stimuli and act as a barrier (like your face mask) to protect you and your organs from particulate matter, viruses, and other people’s snot.
Check out the mucosal layer at the top of the lining. (Image)
The role of cytotoxic chemotherapy and radiation is to act like an atomic bomb to kill rapidly dividing cancer cells (review cytotoxic chemotherapy here). Unfortunately, these treatments can also have collateral damage on our healthy cells, inhibiting further renewal. This leads to damage of those epithelial cells of the mucosal lining in the mouth as well as the rest of the GI tract. Hence why this issue is termed mucositis!
If you’re standing, you might want to sit down for this (let’s be honest, you weren’t going to touch that CV anyways). The process for mucositis development is broken down nonlinearly into five stages:
The pathophysiology process for mucositis development
Pathophysiology of Mucositis
The best way I can describe this process is through eating hot food:
Initiation: Imagine eating a bowl of steaming hot soup, fresh from the microwave. You scoop a spoonful of the delicious chicken noodle only to immediately spit it out due to the burning sensation at the roof of your mouth (direct toxicity due to chemotherapy). Your oral cavity is feeling all tingly in response to the burn (oxidative stress), which is further exacerbated upon gulping down a soda on the side.
Upregulation: Over the next 4-5 days, you forget about the burn, but deep down you know it’s the calm before the storm. The insults (chemotherapy) have created an angry mob of pro-inflammatory cytokine molecules, which creates a stressful environment that is prone to DNA damage. This can then result in epithelial cell death.
Signaling & amplification: After the initial soup accident, siren alarms go off to further release signals that amplify damage to the mucosa (activation of cyclooxygenase-2 pathway, angiogenesis, apoptosis).
Ulceration: Seven days out is described as the most symptomatic phase, which is also when blood counts often reach their nadirs (aka lowest values). As you might imagine, low blood counts = poor immune response, thus leaving patients vulnerable to infection. There may be white patches in the mouth upon physical exam, and EVERYTHING consumed is painful, thanks to the macrophages which chew up the damaged tissue and trigger recruitment of even more inflammatory cytokines.
Healing: After reflecting on your mistakes and eating nothing but bland food for the next 2 weeks, your immune system, specifically the white blood cell count, begins to recover as the epithelial cells rebuild themselves upon the damaged tissue. The ulcers heal, your mouth is no longer in pain, and you’re in the Taco Bell drive through ordering a spicy potato soft taco. Life is good.
Identifying Mucositis and Its Risk Factors
Oral mucositis affects nonkeratinized mucosa on the roof and floor of the mouth as well as the cheeks, lips, and top of the tongue. With these damaged locations, patients often complain of pain, difficulty swallowing, and loss of taste.
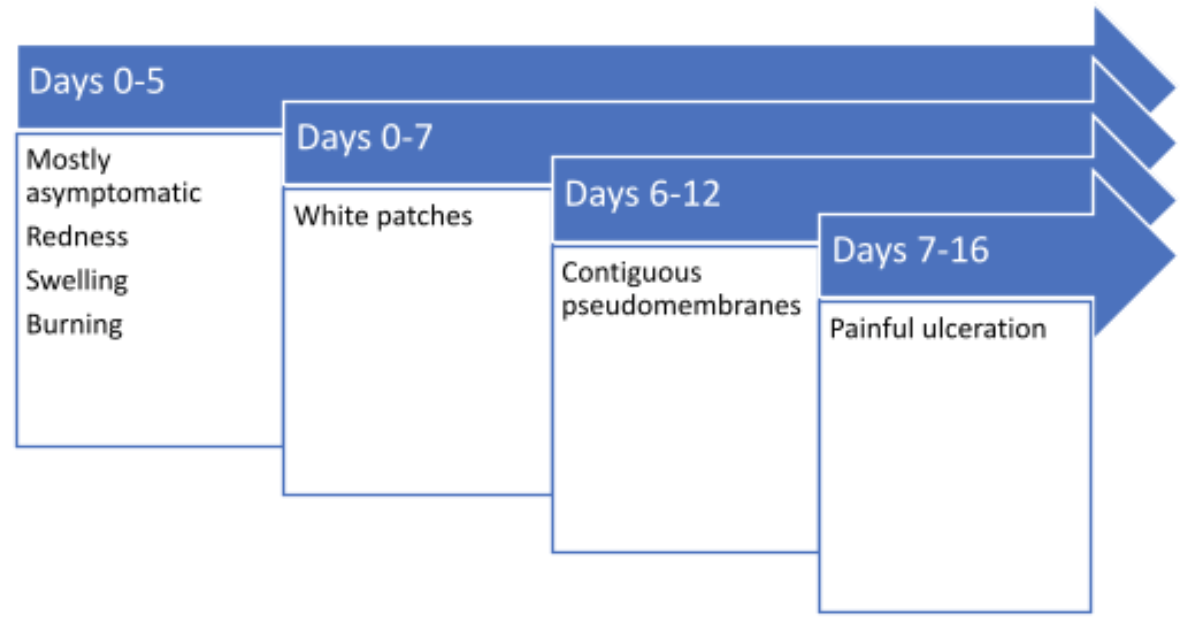
The progression of mucositis over time
Oral mucositis generally begins 5-10 days after chemotherapy initiation and lasts up to 6 weeks (or more). The recovery process tends to coincide with improvement in absolute neutrophil count (ANC) to greater than 500 cells/uL (further ANC discussion here). This is particularly true in the case of hematopoietic stem cell transplant (HSCT), in which recovery of the white blood cells and immune system allows for faster healing.
Gastrointestinal mucositis (GIM) can result from radiation. It presents more often in the small intestine than in the esophagus, stomach, or large intestine. In addition to pain in the area, patients may experience nausea, vomiting, and diarrhea.
Given how miserable this condition can be, it is important to identify risk factors to help prevent as well as reduce the occurrence whenever possible.
Some of the chemotherapy agents that are associated with mucositis are listed in the figure below.
(I wasn’t kidding about the common hallmark toxicity!) So how can we differentiate between agents that have higher risk? A lot of it comes down to:
Drug duration
Strength of the dose
Frequency of administration
Concomitant medications
Typically, prolonged or repetitive lower doses, as well as increased number of cycles, can increase the risk. If a patient has poor kidney or liver function, this can increase susceptibility due to decreased clearance of toxic medications. In addition, risk can increase with previous episodes of mucositis.
Now you may be wondering, “What is hematopoietic stem cell transplant (HSCT) conditioning, and why does this regimen cause such a high incidence of mucositis?” In short, a hematopoietic stem cell is essentially a cell that is commonly isolated from the blood or the bone marrow (found within the spongy part of your bones). These cells can further mature and transform into our various blood cells (white blood cells, red blood cells, and platelets).
(Image)
The role of high-dose chemotherapy in blood tumors is to blast the cancer with the strongest dose in hopes of a curative outcome.
BUT this also wipes out all of a patient’s blood cells, leaving patients vulnerable to infection due to a compromised immune system. In order to speed patients’ recovery times after the conditioning chemotherapy, hematopoietic stem cells are infused to help rescue the bone marrow.
Where do the stem cells come from, you ask? There are different sources to obtain these cells, such as the bone marrow, peripheral blood, and even umbilical cord. They can also be taken from the patient themselves (autologous) or from a donor (allogenic). (Shameless plug: register to be a bone marrow donor here in addition to being an organ donor!)
Radiation therapy is another method used to kill cancer cells using beams of intense energy from a machine outside of the body. The combination of radiation with chemotherapy increases the risk of mucositis. Again, stratification of that risk is dependent on the dose, dose intensity, radiation source, and volume of mucosa irradiated. But nearly all patients who receive radiation for head and neck cancer will likely develop mucositis.
Alright, we’ve discussed some treatment-related risk factors, but are there patient-specific factors that put some people at higher risk than others? You betcha.
Patient-related risk factors for mucositis:
Autoimmune disorders
Diabetes
Caucasians (higher risk than African Americans)
Genetic predisposition to tissue damage
Folic acid or vitamin B12 deficiency
Describing Severity of Mucositis
So how do we measure the severity of oral mucositis?
Due to their ease of use as well as their acceptance by regulatory authorities around the world, the two most commonly used assessment scales are these:
World Health Organization (WHO) scale
National Cancer Institute (NCI)/ Common Terminology Criteria for Adverse Events (NCI/CTCAE v.3.0) scale
Unfortunately, there is not a validated scale that is published for assessing GI mucositis.
Mucositis Prevention Strategies
You may not be able to completely stop mucositis, but there are ways to help mitigate the side effects and complications. I encourage you to check out the Mucositis guidelines developed by the Mucositis Study Group of the Multinational Association of Supportive Care in Cancer (MASCC) and the International Society of Oral Oncology Guideline here.
Oral Mucositis
Before we dive head first in prevention of oral mucositis, you should know that a lot of the prophylaxis studies were done in head and neck cancer patients due to the high incidence of mucositis in this population. Therefore, guidelines state that recommendations should not be extrapolated to other populations unless otherwise noted.
With that said, the following are prevention strategies for patients receiving head and neck radiation therapy:
Oral care protocols
Benzydamine hydrochloride
Low level laser therapy (LLLT)
For patients receiving systemic chemotherapy, the guidelines include:
Oral care protocols
Oral cryotherapy
Palifermin
LLLT
Oral Care Protocols
They say the mouth is the gateway to overall health. Therefore, a good oral care regimen is important to help decrease the severity of mucositis and prevent infection from open sores.
And good news! The patient is likely to have all the supplies lying around their home!
Oral rinses
The mainstay for an oral care regimen is a mouth rinse, and it has been supported by several studies that good ol’ salt water is not only effective but also affordable. The secret formula for the salt rinse is 1 teaspoon of table salt to 1 quart of water, and patients should swish and spit before and after meals as well as at bedtime. The rationale of the mouth rinse is to help remove any debris or particles in the mouth, in addition to lubricating and cleaning the oral cavity. Staying hydrated is also very important!
Brushing
Another important aspect of oral care is educating patients on oral hygiene and proper brushing techniques. This includes brushing with a soft bristle toothbrush 2-3 times a day, avoiding mouthwashes with alcohol or products that may irritate the mouth, and avoiding toothpastes with whitening agents.
Flossing
Patients should floss at least once daily. The exception to this is if a patient has significant thrombocytopenia when the platelet count is less than 50,000, which could predispose them to bleeding with flossing. Also, if bleeding occurs during flossing and lasts more than 2 minutes, flossing may not be the best idea.
Dentures
If your patient wears dentures, they should remove them whenever possible to let the gums breathe. They should also not be worn if mouth sores are severe.
Foods
Patients should be advised to avoid any food or drinks that may exacerbate their sores, such as alcohol and spicy, hot, or acidic foods (this includes Taco Bell’s spicy potato soft taco, sorry).
Palifermin
Palifermin (Kepivance®), is a keratinocyte growth factor-1 (KGF). It works to protect the oral mucosa by binding to the KGF receptor, which is present on epithelial cells of the tongue as well as other organs, and stimulates epithelial cell proliferation and differentiation. The drug is dosed at 60 mcg/kg/day IV for 3 days before the conditioning regimen and 3 days after HSCT for the prevention of oral mucositis. It is important to give the third dose 24-48 hours before the conditioning treatment as giving it within 24 hours may actually increase the severity and duration of oral mucositis.
Now why is that?
Recall that the chemotherapy targets rapidly dividing cells, and the mechanism of palifermin is to stimulate epithelial cell renewal. So the stimulated cell renewal might inadvertently catch the attention of the chemotherapy, leading to increased risk for mucositis.
Sometimes, timing really is everything.
Palifermin is only indicated for use in patients with blood cancers receiving high-dose chemotherapy + total body irradiation (TBI) for autologous HSCT. It may also be considered for those undergoing myeloablative conditioning TBI prior to allogenic HSCT. However, it is not recommended for regimens in the absence of TBI.
Benzydamine
This drug wears many hats in that it has several roles to help prevent oral mucositis. It has anti-inflammatory, anesthetic, analgesic, antipyretic, and antimicrobial properties. This is sounding a lot like an NSAID, doesn’t it? That’s because it is!
But unlike other NSAIDs, benzydamine does not inhibit cyclooxygenases (COX); rather, it stabilizes membranes, resulting in local anesthesia. It also inhibits production of pro-inflammatory cytokines (TNF-alpha and IL-1beta). The agent is used as a mouthwash rinse in patients receiving moderate-dose head and neck radiation (<50 Gy).
Currently, this drug is not commercially available in the United States, although it may be prepared by some compounding pharmacies. Furthermore, the use of this agent by guidelines is a suggestion rather than a recommendation due to inadequate evidence.
Lower Level Laser Therapy
LLLT is exactly what you think it is. It involves focusing low-energy laser beams to affected tissue and is thought to work by stimulating certain cells that help speed up the healing process. Now how does it do all of this? Pop quiz: what is the powerhouse of the cell?
I’m hoping you answered mitochondria. Recall that the mitochondria is involved in all of those processes mentioned above. But when the mitochondria is placed in a stressful environment, it produces nitric oxide, which binds to cytochrome c oxidase, and displaces oxygen. This leads to reduced ATP, increased inflammation, and poor cellular function. The light therapy at low intensity applied to those stressed tissues is absorbed by the cytochrome c oxidase and also displaces the nitric oxide, which helps to restore balance.
There is currently a lack of guidance for laser parameters and LLLT schedules as clinical practice varies among institutions. Current mucositis supportive care guidelines recommend that this therapeutic modality is for patients receiving high-dose chemotherapy with or without TBI as conditioning for HSCT. It’s also suggested for those receiving radiation for head and neck cancer.
Cryotherapy
You after your 3rd popsicle and only 10 minutes in…20 minutes to go. (Image)
Contrary to popular belief, this actually has nothing to do with crying. It actually involves sucking on ice chips, which causes vasoconstriction and helps to decrease exposure of the oral cavity to the cytotoxic chemotherapy. Thirty minutes of oral cryotherapy is recommended for patients receiving 5-FU bolus therapy and is suggested for high-dose melphalan.
GI Mucositis
Prevention modalities used for GI mucositis include:
Amifostine
Sulfasalazine
Probiotics containing Lactobacillus
Amifostine
Amifostine (Ethyol®) is a prodrug metabolized by an enzyme to a free thiol metabolite that binds to reactive metabolite of the chemotherapy or radiation and reduces the cytotoxic effects. It is recommended by guidelines to prevent radiation-induced proctitis and is suggested to prevent esophagitis after chemoradiation for non-small cell lung cancer (NSCLC). The drug is administered as 340 mg/m2 IV over 3 minutes before radiation to prevent radiation-induced proctitis, and given as 500 mg IV twice weekly before radiation to prevent esophagitis after chemoradiation in non-small cell lung cancer NSCLC.
This chemoprotective agent has one adverse effect to be aware of, which is nausea.
Sulfasalazine
Sulfasalazine is a medication that can help reduce inflammation of the GI tract in patients undergoing pelvic radiation.
It’s not totally clear how sulfasalazine works to reduce inflammation, but one theory is that it (or its metabolites 5-aminosalicylic acid and sulfapyridine) may work locally in the lower GI tract as an anti-inflammatory. The recommended dosing is 500 mg PO twice daily to prevent radiation-induced enteropathy after pelvic radiation. It is currently considered a suggested option by the MASCC guidelines for prevention of GI mucositis.
What if patient has a sulfa allergy? People who are allergic to sulfa drugs may react to sulfasalazine and should therefore avoid use.
Probiotics
“Hold up. Aren’t probiotics a type of bacteria? I thought we were trying to prevent infection?”
Actually, the microorganisms in probiotics are friendly and are often taken to help colonize the gut with good microorganisms, similar to your normal flora. If you didn’t know, they are also present in food that you might eat every day like yogurt or sauerkraut.
The most common probiotic bacteria are Lactobacillus and Bifidobacteria. Different probiotics address different health conditions, which is why selecting the right product is essential.
Specifically, Lactobacillus acidophilus was observed in studies to reduce inflammatory cytokines caused by 5-FU damage to the intestinal mucosa (more on the probiotic is described in this study here.)
So what is its role in preventing GI mucositis?
Like previously mentioned, your gut is comprised of a complex eco-system of different healthy bacterial species. They all play roles in important health functions, such as manufacturing vitamins, turning fibers into short-chain fats, as well as helping stimulate the immune system and strengthening the gut wall (remember symptoms of GI mucositis include nausea, vomiting, and diarrhea, which can be fairly traumatic on the gut!).
Therefore, guidelines suggest the use of probiotics containing Lactobacillus to prevent life-threatening diarrhea after chemoradiation in pelvic tumors.
Treatment of Mucositis
Hang tight, we’re in the home stretch!
So your patient is presenting post chemotherapy with oral lesions, and she states she is in pain. A LOT OF PAIN.
Pain is a significant issue with oral mucositis, and it affects patients’ nutrition and overall quality of life. Thus, the cornerstone of treatment for oral mucositis is targeting this specific symptom.
To remedy this issue, there are various mouth rinses available that are suggested by the guidelines including 2% morphine and 0.5% doxepin.
Doxepin? Like the tricyclic antidepressant doxepin?
Doxepin rinses have been observed to relieve pain from oral mucositis in studies and found to improve the symptoms over a 4 hour period. It carries anesthetic and analgesic benefits when applied topically but has expected side effects such as drowsiness.
If the pain is severe enough, meaning grade 3 or 4, requiring admission due to limited oral intake, you are going to need something stronger than a topical magic mouthwash. The patient is likely going to be started on IV fluids and systemic opioids. The guidelines recommend imitating patient-controlled analgesia with morphine for HSCT patients.
One important thing to note is that, if a patient is able to tolerate oral opioids, be cautious about any combination products that contain acetaminophen. Because what’s likely happening while these patients have mucositis? Probably neutropenia. And if they are taking oxycodone + acetaminophen around the clock, that acetaminophen might mask a fever which is the main (if not only) symptom to monitor for febrile neutropenia.
The treatment is somewhat limited for GI mucositis, and guidelines suggest options such as sucralfate enemas or hyperbaric oxygen.
The tl;dr of Mucositis
Cytotoxic chemotherapy and radiation can cause mucositis, which affects the oral cavity all the way through the end of the GI tract.
Complications from mucositis include pain, nutritional problems, and increased infection risk.
A simple and cheap preventive measure for both oral and GI mucositis is maintaining proper oral hygiene.
Treatment of mucositis often involves optimal pain control and topical mouth rinses.
Finally, avoid spicy potato soft tacos and hot chicken noodle soup. It may be good for the soul, but it’s not always good for the mucosa. ✍ ✍ ✍ ✍