Pharmacology 101: An Overview of Statins
Steph’s Note: Today we introduce the start of our Pharmacology 101 series. These posts will be the “everything you need to know - or forgot you knew - about big ticket classes of medications”. They will NOT be a regurgitation of the information you can find in the monograph, promise! Let’s give that info some context, yay?
Whether you’re a first year pharmacy school student or a veteran pharmacist, we hope to bring you the highlights. We want to either give you the baseline you need for moving forward or perhaps fill some knowledge gaps for info you haven’t used in a while.
As Prince John would say, “Either way, we oughta have a lotta fun!”
Because after all, this is tl;dr pharmacy.
BTW - We compiled ALL of our Pharmacology 101 posts into one handy, downloadable (and printer-friendly) PDF. You can get your copy of it here.
What is Cholesterol?
Cholesterol is bacon!! Bacon!!! BACON!!!!
Sorry, got distracted.
Cholesterol is an organic, fatty substance used in multiple natural body processes. For example, it helps to compose and stabilize cell walls and is used to synthesize substances like steroid hormones (corticosteroids, androgens, estrogens, etc.) and bile acids.
But of course we all know cholesterol from the media as a bad thing. No matter how delicious bacon is.
Too much cholesterol circulating in the blood can build up and develop into fatty streaks on the sides of blood vessels, which leads to plaque formation and eventual vessel narrowing, aka atherosclerosis. Atherosclerosis and subsequent plaque rupture is implicated in multiple cardiovascular disease states, including coronary artery disease (e.g., heart attacks or myocardial infarctions) and cerebrovascular disease (e.g., strokes or cerebrovascular accidents).
How do we know if a patient has too much cholesterol in the blood?
Well, we can’t really directly measure the true amount of cholesterol in a person’s body.
Instead, we use indirect measures of the proteins responsible for transporting cholesterol. These proteins are called lipoproteins since they consist of both lipid and protein components. The lipid components include cholesterol and triglycerides. The proteins include apolipoproteins, which provide structure to the transportation molecule and also may help with processes like receptor binding.
Structure of a lipoprotein. See how free cholesterol can help with maintaining structure in-between the phospholipids, but then esterifed cholesterol (with fatty acids) is contained inside. (Image)
You can think of these lipoproteins as little spheres of juicy cholesterol and triglyceride cargo surrounded by a protein and phospholipid coating, zooming around the blood until picked up by a receptor (or perhaps by a growing plaque).
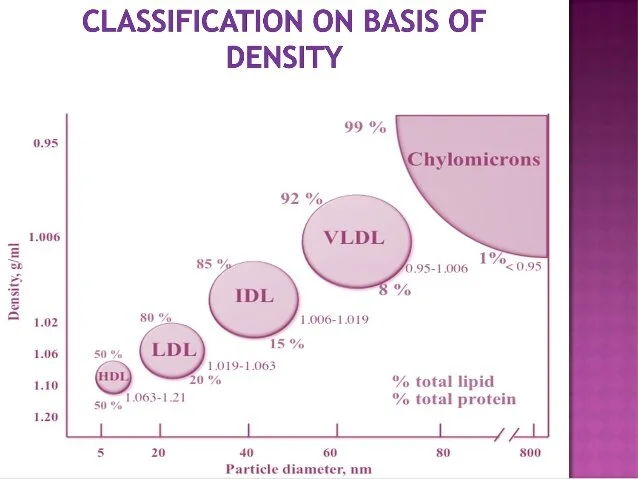
There are several types of lipoproteins that differ in their relative compositions, including:
chylomicrons
very low density lipoprotein (VLDL)
intermediate density lipoprotein (IDL)
low density lipoprotein (LDL), and
high density lipoprotein (HDL).
See how the rather small HDL particle has a lower lipid to protein ratio compared to the ginormous, looming chylomicron that is almost all fat? (Image)
HDL has a lipid to protein ratio of about 1:1, whereas in contrast, chylomicrons are about 99:1! LDL is about 4:1. Functionally, this means HDL is much more compact than the other, fattier particles.
Other than hearing about how bad cholesterol is in general, we always hear in the media how HDL is “good” cholesterol and LDL is “bad” cholesterol. But this is kind of misleading. Cholesterol just…is.
When we hear those terms of good and bad, it’s really more related to the functions of those cholesterol transporters.
HDL is involved in reverse cholesterol transport, meaning it is able to take on excess cholesterol from peripheral tissues and transport it back to the liver for metabolism and excretion. This is why it is known as “good” cholesterol.
LDL particles transport cholesterol to cells in the body that need it. Although this is a necessary process, their good intent can be twisted when there’s too many of them. Or they get distracted by the plaque party, make a pitstop at the blood vessel wall, and never leave.
So how can we improve the ratio of good HDL to bad LDL cholesterol transportation and thereby prevent the dreaded atherosclerotic cardiovascular disease (ASCVD)?
Enter the statins.
What are Statins?
Statin medications lower cholesterol levels by decreasing cholesterol production. The name “statin” is actually a nickname for the HMG CoA reductase inhibitors (because who wants to say that mouthful all the time).
But if we really want to understand how this class of medications work, it’s important to remember the more technical name.
And just for fun, let’s get a little more technical. “HMG CoA reductase inhibitor” is also a bit of a nickname. It stands for 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitor.
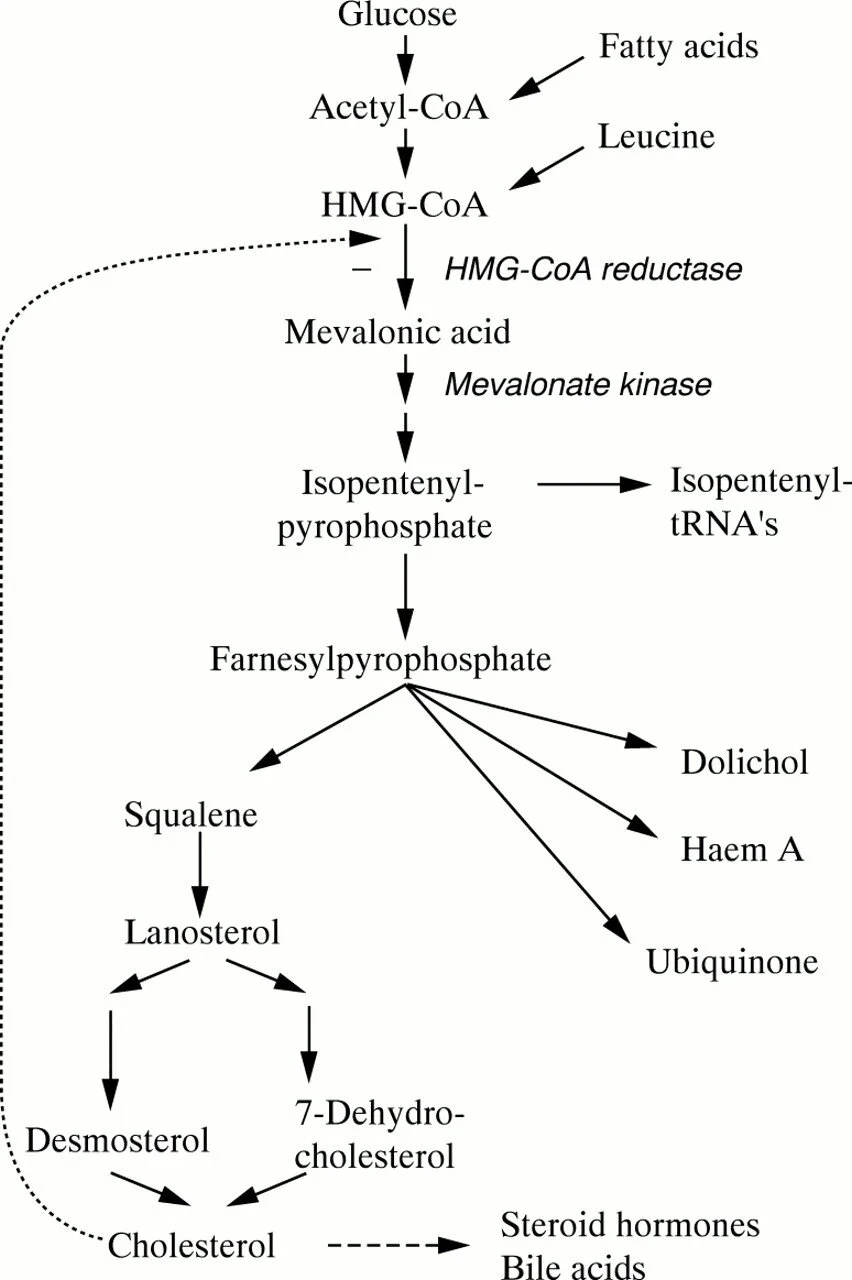
Here’s a quick review of cholesterol biosynthesis. Pay special attention to the conversion of HMG-CoA to mevalonic acid. This is the rate-limiting step in cholesterol synthesis, and it’s catalyzed by the enzyme HMG-CoA reductase. (Image)
Back to biochem for a moment now. HMG-CoA reductase is the enzyme responsible for a pivotal role - nay, the rate-limiting step - in hepatic cholesterol synthesis. This important step is the conversion of HMG-CoA to mevalonic acid.
See to the left for a quick review of this process.
Because statin medications have a similar chemical side group to HMG-CoA, they are able to mimic HMG-CoA reductase’s normal substrate and competitively inhibit production of mevalonic acid. This effectively short circuits the downstream production of cholesterol.
VLDL and IDL are heavy in triglycerides. They also have some of the same proteins on their surfaces as LDL, which may account for why they are recognized and snapped up by hepatic LDL receptors. And voila, fewer circulating triglycerides! (Image)
Because of this decreased internal hepatic cholesterol synthesis, hepatocytes respond by upregulating production and decreasing breakdown of their surface LDL receptors. This leads to increased hepatocytes binding of LDL circulating in the blood.
The end result?
Increased numbers of cholesterol-containing LDL particles are removed from the blood by hepatocytes, leaving less cholesterol to contribute to atherosclerosis!
So how do statins decrease triglycerides too, since triglycerides aren’t substrates of the LDL receptors?
The answer to this goes back to some of the other lipoproteins. VLDL and IDL are precursors to LDL and so share some of the same surface proteins as their most-wanted-for-capture descendant. So when those upregulated LDL receptors are snapping up LDL out of the crowd, they also increase removal of VLDL and IDL. Because the latter are rather rich in triglyceride cargo, removing them from the circulation also removes a pretty significant number of triglycerides.
Where did Statins Come From?
A little bit of history sometimes goes a long ways for remembering drug information, so here’s the history lesson today:
Find the fungus among us.
Like so many other medications, statins originally derived from mold. They were isolated from Penicillium citrinum in 1976. (Not to be confused with the source of penicillin, Penicillium chrysogenum. But mold, nonetheless.)
The first “true” statin studied in humans was named compactin. Doesn’t exactly have a great ring to it, does it? Sounds like a bowel med, if we’re being honest. So they renamed it to mevastatin, which is only slightly better, but at least it has the recognizable “statin” on the end. Mevastatin was never FDA approved.
The first FDA approved statin was lovastatin, patented by Merck in 1979 and approved for medical use in 1987. It was from a different fungus, Aspergillus terreus. And from there, lovastatin’s cousins since then are either chemically modified versions of itself or synthetic compounds.
Long story short, if you want to make a buck, maybe take a second look at that moldy orange in your fridge…
Kidding. Please throw it out and scrub a little bleach around. Didn’t your parents teach you not to play with gross things? Geez!
Which Medications are in the Statin Family?
Currently, there are 7 statin medications on the market. Each has slightly different properties in terms of how they impact the various lipoprotein levels and also triglyceride levels. Picking which one is most appropriate for your patients depends on many factors, including what their estimated ASCVD risk is (a whole other discussion), cost, tolerance of any adverse effects, and concomitant medications.
Let’s take each of these pieces individually.
Relative Statin Potency
For statin potency, I want you to remember RASLPF. Or as I hear it in my head, “Razzle-puff.” (Shout out to Jackie, my PY3 lab teaching assistance who taught us this, since it has always stuck with me!) In terms of LDL-lowering ability, from most to least potent, here are the statins:
Rosuvastatin (Crestor)
Atorvastatin (Lipitor)
Simvastatin (Zocor)
Lovastatin (Mevacor)
Pravastatin (Pravachol)
Fluvastatin (Lescol)
But wait a minute… That’s only 6 medications? Didn’t I say there are 7?
Oh yeah, I guess we shouldn’t forget about pitavastatin (Livalo). Pitavastatin was the most recently approved statin medication (2009). In terms of potency, it falls somewhere between lovastatin and pravastatin. So I guess you could make it RASL(P)PF or “razzle-puh-puff”…
But it sort of kills the ring, right?
Plus, given pitavastatin didn’t really add anything all that special to the statin options AND it’s brand name ($$) only, it’s not really highly utilized.
But here’s a statin intensity chart that summarizes dosing and potency. It actually does include pitavastatin just in case you ever do need it as an option:
(Image)
And BTW, to help you figure out where statins (and every other lipid therapy) fit in the treatment landscape, check out our Hyperlipidemia Cheat Sheet. It’s packed with dosing info, drug interactions, clinical pearls, and all sorts of other goodies (including a breakdown of all EIGHT(?!) formulations of fenofibrate). And yes, you’d better believe it includes a statin intensity chart.
Adverse Effects of Statins
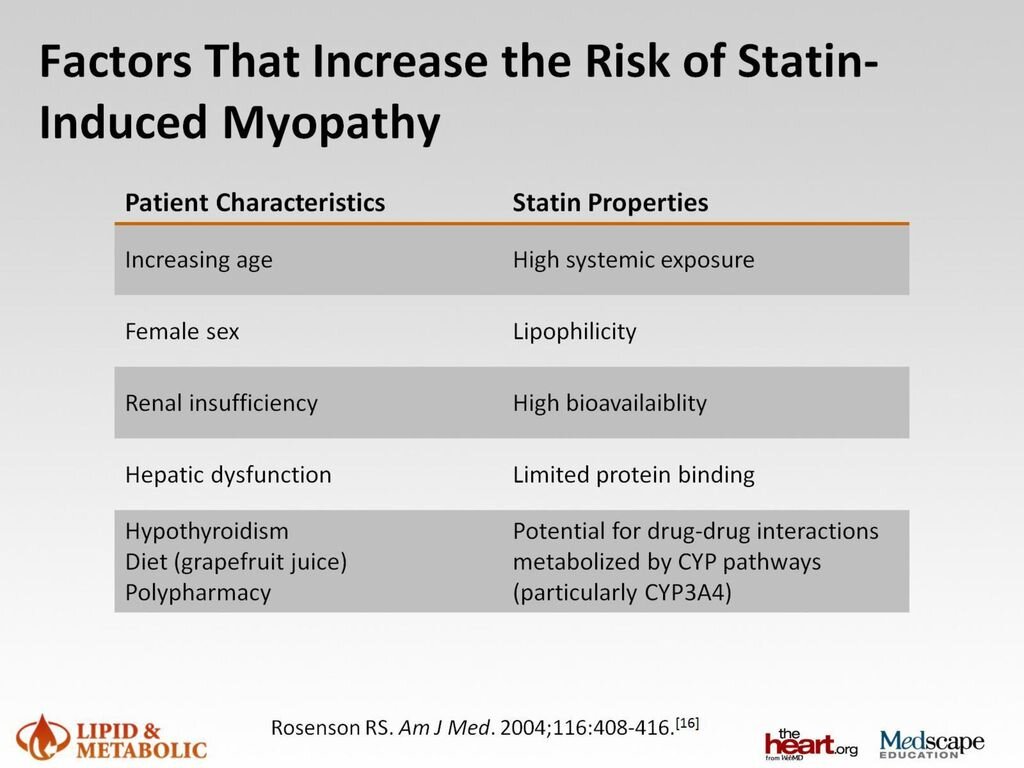
Muscle toxicity is one of the most widely recognized adverse effects of statin therapy, but it’s also a bit of a chameleon. It can manifest as anything from mild muscle aches (aka myalgia or myopathy) with an elevated creatinine kinase (CK) level to something as severe as rhabdomyolysis or immune mediated necrotizing myopathy (IMNM).
Myalgias and mild CK elevations (<5x the upper limit of normal) may occur in 10-20% of statin-treated patients, whereas rhabdomyolysis has an incidence of 1 in 100,000 patients - much more rare! IMNM, an autoimmune myopathy, has been observed in ~2-3 patients in 100,000, so also very rare.
(Image)
Like any other adverse effect, however, we should be thinking on an individualized basis for what may predispose our patients to this toxicity. Check out the list of risk factors in the table to the right.
How do statin-induced myalgias present for patients?
When it comes to myalgia and CK elevations, most patients complain of aches in their calves and thighs although they can occur in additional muscles as well. The key here is that these are usually unexplained muscle aches.
We’re not really talking about every muscle ache a patient has after working in the yard for 5 hours! But if a person begins to notice persistent aches without a causative factor, perhaps it’s time to eyeball the statin.
So what should we do if a patient does complain of these symptoms?
First, of course we want to rule out more serious disease processes, including rhabdomyolysis (check that renal function!). Second, a full patient history should be obtained to determine if there are any other explanations for the muscle aches or that may cause elevated statin exposure beyond the norm.
Was the patient started on an interacting medication that inhibits statin metabolism? Statins are CYP3A4 and CYP2C9 substrates, so just consider ALL the possible drug interactions with CYP3A4 and CYP2C9 inhibitors! (Be sure to check out our post on how to do a med rec to help you get an accurate medication history).
Did the patient decide to go on a diet and eat grapefruit every day for breakfast? Did they switch to low calorie Fresca soda? Sure, seems like a healthy choice until you, the pharmacist, consider ALL the foods that contain grapefruit!!
Yeah, I know. But you try to find a google image of killer grapefruit! Sorry, best I can do is killer pears, but they’re pretty mean looking, true? (Image)
There are a few very important counseling points there. First, patients should check with a pharmacist if they start or stop any new medications. (Every patient should be told this whenever possible.)
Second, beware the grapefruit. Other popular citrus fruits like lemon, lime, and orange are ok. But that grapefruit interferes with CYP3A4 metabolism.
Baaaaaaad grapefruit.
If it does appear to be a case a mild myalgias with or without CK elevations, you have a couple of choices:
Continue the same statin.
These mild aches and pains and even mild CK elevations are not life-threatening. Some patients improve with time even without changing therapy.
Try to address other modifiable risk factors, such as potential drug interactions or grapefruit consumption.
Of course, as expected, when trying to explain the power-through option to the people living the statin life, this isn’t exactly the most popular of suggestions, which is totally understandable. Would you want to deal with feeling crappy, especially when we have other medication choices?
Try a different statin.
Sometimes even changing to a different statin can ameliorate the myalgias. Not all statins are created equally, and even though they share a similar HMG CoA doppelgänger side chain, they do have different physicochemical properties. See below:
Even though it’s tempting to treat them all equally, statins are different medications. So be a good, type A pharmacist, and check those details :) (Image)
Which of these properties seem to matter most for causing myopathies? Bioavailability and lipophilicity. The more lipophilic and bioavailable, the higher tendency for causing muscle toxicity. So if you have a patient who needs a high intensity statin but is experiencing muscle aches on atorvastatin, try switching to an equivalent dose of rosuvastatin. (Remember that potency chart from earlier? This is where it is MAJORLY useful.)
Also consider, however, that drug and food interactions can alter the patient’s actual exposure to statins. So just because a person is on a statin that should theoretically be lower risk, that doesn’t mean adverse effects can’t and won’t happen.
Oh yeah, and there is a third option for what to do if your patient is experiencing myalgias with statins:
Discontinue statins altogether.
Obviously, this is not really ideal. We start our patients on these medications (hopefully) for good reasons, so nixing an entire class of medications, especially one that has been proven so stinking useful, is a last resort.
Often, the patients are the ones who make this decision for us. After all, once they’ve run through a couple different statins without improvement in their aches and pains, sometimes patients swear off any further statins. From a quality of life perspective, it’s understandable. From a clinician’s perspective, sometimes it’s hard to see “statins” on the allergy list when perhaps you just haven’t quite come across the right one for the patient.
On a positive note, at least these days there are other classes of medications to help lower cholesterol and ASCVD risk. Check out this post on PCSK9 inhibitors.
Moving on from muscle toxicity.
To give a statin, or not to give a statin…? That is the question! (But really, usually there’s not too much of a question.) (Image)
Statin Controversies
There has been some controversy in the past about whether statins cause reversible memory impairment and/or worsening cognition. The latest body of evidence on this consideration is a 2019 report from 6 years’ worth of observational data, in which statins did not appear to worsen memory or cognition.
There has also been some controversy surrounding statin therapy increasing risk of diabetes. Seems a little counterintuitive considering having diabetes qualifies patients for moderate or high intensity statin therapy, right? And we have evidence that statins lower ASCVD risk in patients with diabetes. So what do we do?
Really, if a patient is high enough risk to warrant statin therapy either as primary or secondary ASCVD prevention, usually we initiate the statin and monitor blood glucose levels. The benefits of statin therapy have been proven time and again, so the benefits generally outweigh the risks in this scenario.
Ok, you have officially made it to the end of statin pharmacology! Hopefully this review spurs you to investigate more about this highly utilized class of medications and/or it filled in some knowledge gaps. Either way, enjoy your bacon - just not toooo much!!
And BTW, to help you figure out where statins (and every other lipid therapy) fit in the treatment landscape, check out our Hyperlipidemia Cheat Sheet. It’s packed with dosing info, drug interactions, clinical pearls, and all sorts of other goodies (including a breakdown of all EIGHT(?!) formulations of fenofibrate). And yes, you’d better believe it includes a statin intensity chart.