Heart Failure Part 1: Background and Pathophysiology
This article has been reviewed and is up-to-date as of 08/07/2024.
Brandon’s Note: J. Nile Barnes, PharmD, BCPS is a Clinical Assistant Professor of Health Outcomes and Pharmacy Practice at the University of Texas at Austin College of Pharmacy. He's also a clinical pharmacist for an academic medical center. Prior to becoming a pharmacist, he spent several years as a paramedic.
Basically, he's got hands on experience with most levels of medical practice and education. And he's kind enough to share that experience with us all.
The following is Part 1 of an (excellent) 3 part series on heart failure. Dr. Barnes will tackle background and pathophysiology here; before moving on to signs and symptoms and then pharmacotherapy.
As an FYI, you can get all 3 posts in this series as one downloadable (and printer-friendly!) PDF. PDF currently under construction as this series is being updated!
Heart failure (HF) strikes fear in the eyes of most pharmacy students; I think mainly because there are so many drugs and so many moving parts to this. Let’s break it down to basics.
This post will cover some normal heart physiology and some HF pathophysiology. My next two posts will cover signs and symptoms and pharmacotherapy.
If you don't recall how the cardiac cycle works, here is a great visualization:
Heart Failure Pathophysiology
HF is simply the inability of the heart to pump blood forward. Understanding the hemodynamics of the cardiac cycle is the first step to understanding HF.
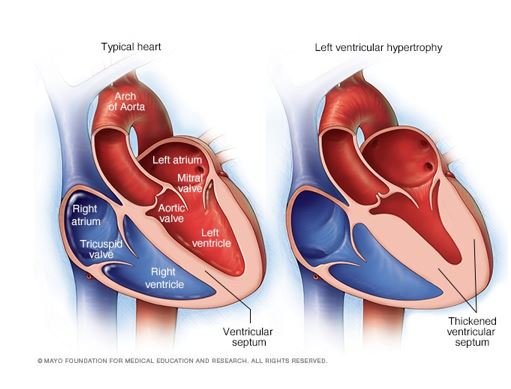
Here is a cutaway of a heart:
Courtesy of the Cleveland Clinic.
You can see all four chambers and a bit of the aorta cut open. You should know all four of the chamber names.
The heart is really TWO pumps with a common wall (the interventricular septum): the left heart and the right heart. And in fact, they both have booster pumps (the atria) to help things along.
This is incredibly important to remember when we are talking about HF. Sometimes the primary failure is on the left, other times it is on the right. Left heart failure can cause right heart failure, too!
Let’s take a moment to remember where the left heart gets its blood and the where it pumps it to. The left heart receives blood from the lungs via the four pulmonary veins. These drain into the left atrium (LA), then through the mitral valve into the left ventricle (LV).
Then the heart contracts and sets off a series of events. The LA contracts, boosting the filling of the LV. The LV then ejects most of its volume out through the aortic valve into the aorta delivering it to the body. The pressure on the systemic side is what is reflected in the blood pressure we get from the arm (or other systemic site).
A typical blood pressure reading of 120/80 represents the pressure when the left heart contracts (known as systole which is about 120 mm of mercury or mmHg), and the pressure when the left heart relaxes (diastole which is about 80 mmHg). It takes this kind of pressure to pump blood against gravity into the head and systemic circulation.
The story is just about the same from the right side. The right heart gets its blood from the inferior and superior vena cavae. Like the left side, this is primarily passive return to the heart.
The passive return of blood drains through the right atrium (RA) through the tricuspid valve into the right ventricle (RV). Then the heart contracts and sets off another series of events. The RA contracts, boosting the filling of the RV. The RV then ejects most of its volume out through the pulmonic valve into the pulmonary trunk delivering it to the lungs.
The pressures on the right side are SUBSTANTIALLY LOWER! The right heart only has to pump to the lungs, which are much closer and therefore require less effort. When we measure these pressures the numbers are more like 25/9 mmHg.
So I mentioned that HF is the inability of the heart to pump blood forward. How does that work?
Let’s just look at the left heart for now. As mentioned above, blood flows into the LV from the LA. Let’s imagine the left end-diastolic volume for a patient is 140 mL.
That means that when the atrium has finished contracting and boosting the ventricular volume, there is about 140 mL in the ventricle. If the ejection fraction (EF) is 65%, then 65% of 140 mL (about 91 mL) is ejected.
ventricular volume x EF = ejection volume
140 mL x 65% = 91 mL
These are normal values. What can upset this?
Anything that interferes with either filling the ventricle or squeezing the blood out.
So, Hans and Franz have such big biceps in this video that they cannot move their muscles through a full range of motion.
The same thing can happen to the heart. Untreated hypertension (HTN) can result in left ventricular hypertrophy (LVH) which can decrease the ventricular volume as the muscle grows inwards as well as outwards.
This means the maximum ventricular volume may drop. If we use the example in the previous paragraph, the 140 mL volume may be decreased (let’s say to 86 mL). If the EF is preserved at 65%, the new ejection volume is now 56 mL.
86 mL x 65% = 56 mL
Courtesy of Mayo Clinic.
A 40% decrease in ejection volume with no change in EF. This is now called HFpEF (heart failure with preserved ejection fraction). It was formerly called diastolic failure or diastolic dysfunction because the filling process (diastole) is impaired.
Instead of Hans and Franz, let’s now say the patient is having (or has had) a large left ventricular wall myocardial infarction (MI), like Fred Sanford always claimed in the 1970s.
If this myocardial muscle tissue is now dead or dying, it will not contract, and it will stretch and can thin or balloon out. This weakened muscle cannot squeeze as hard and will result in failure also.
Let’s say our end diastolic volume is back to normal (140 mL). But now we have a decrease in systolic effort (the squeeze), and let’s say it is now 40%. Forty percent of 140 mL is going to 56 mL.
Again, this patient has a decrease of ejection volume to 56 mL, but this is due to the reduction in EF and there is a normal end-diastolic volume (before the squeeze).
140 mL x 40% = 56 mL
Also courtesy of Mayo Clinic.
This is now known as HFrEF (heart failure with reduced ejection fraction). It was previously called systolic failure since the systolic effort was decreased. An EF of less than or equal to 40% is generally the definition of HFrEF.
I hope you noticed the ejection volume was the same in both examples! Both cause the same loss of ejection volume, but diastolic failure (HFpEF) does it by decreasing ventricular filling volume and systolic failure (HFrEF) does it by decreasing ventricular squeezing force.
And just to be contrary, patients can have BOTH systolic and diastolic dysfunctions. Imagine the patient with longstanding HTN that has developed diastolic (HFpEF) dysfunction who now has a massive heart attack.
He started with a poor end-diastolic filling, and now has a reduced systolic squeeze. This is a set-up for rapid decline, and possibly death!
Summary
Two of my mentors are retired army colonels (shout out to Lt Col. Bob and Col. Jim). They always taught every topic in the “Army Way.” The army got it from Dale Carnegie who got it from Aristotle. That format is:
Tell them what you are going to tell them. Introduce the topic.
Tell them. Give them what you’ve got.
Tell them what you told them. Summarize the high points.
So, here is the summary:
We defined HF as the inability of the heart to pump blood forward.
We described HF as affecting the left or right heart.
We described HF as either having reduced or preserved EF (or both).
If you didn’t get these three things out of this post, shoot us an email!
The set-up for the next installment:
In the next post, I will talk about the signs and symptoms of HF.
BTW, I hope you also noticed that I have not said “CHF” at all throughout this post. The “C” in CHF properly stands for “congestive”. Not all patients have congestive signs and symptoms, so this is NOT an appropriate abbreviation anymore (but is still accepted by the payors).
If you find yourself using it or are confused because others have used it, substitute the word “CHRONIC” for congestive. Chronic heart failure = heart failure. Unless we are talking about acute decompensated HF (ADHF)... But that is a topic for another time.
Oh, just a side note, signs and symptoms should really be symptoms and signs. We always give subjective data before objective data, so the symptoms (subjective) should be listed before the signs (objective).
But history has us saying it the other way around and, if you have heard it enough as “signs and symptoms,” it just sounds odd to say “symptoms and signs.”
Get this Series as a PDF!
Want a printer-friendly version of the ENTIRE heart failure series? Or do you just want to save the series for offline viewing? You can now get the entire Heart Failure Series as a single (and attractive) PDF. PDF currently under construction as this series is being updated!