Everything You Need to Know about Tumor Lysis Syndrome
Steph’s Note: For this week’s post, you’re in for a treat! No, we’re not gonna ride the COVID train. And you’re right, we just chatted professionalism last time. This go around, we’re hitting the clinical meat! Clinical oncology, to be exact. So who’s going to be broadening our oncology horizons?
Kristin Holbrook is a 2020 graduate of St. Louis College of Pharmacy. Originally from Mountaintop, PA, she obtained her B.S in Chemistry from the University of Pittsburgh before moving to the Midwest to reach her dream of becoming a pharmacist. She has a passion for oncology pharmacy and the drug approval process and enjoys helping others learn these topics too!
Kelley Carlstrom, PharmD, BCOP is a residency-trained oncology pharmacist who is passionate about communicating the value of pharmacists in the care of patients with cancer. She has worked in traditional oncology specialist roles in large academic and small community hospitals but has found a love of non-traditional roles. She wants to encourage other pharmacists to enter oncology specialty practice and offers ways to support that transition. You can learn more at www.KelleyCPharmD.com.
BTW - We compiled ALL of our Oncology Supportive Care posts into one handy, downloadable (and printer-friendly) PDF. You can get your copy of it here.
Managing treatment-related complications is an important role for pharmacists and is particularly true in oncology. Whether you are currently working in oncology, want to be working in it, or are just generally interested in it, there are many ways you can have an impact on this population. Tumor lysis syndrome is one important complication that pharmacists should be knowledgeable about as part of the patient care team. Here you will find an overview of this cancer complication along with prevention and treatment strategies.
What is Tumor Lysis Syndrome?
Simply, tumor lysis syndrome (TLS) is an emergency that can occur in people with cancer. Sounds straightforward, right? But TLS is nothing to take lightly. It can quickly sneak up on patients (like that pharmacology exam tomorrow morning you’ve procrastinated studying for) and can be fatal if not recognized and treated properly.
(Image)
TLS most commonly occurs in patients with blood cancers who are receiving cytotoxic therapy that kills the quickly dividing cancer cells. It can occur in as little as a few hours after treatment but is most frequently seen in the first 2-3 days after treatment begins. It is important to note that, although rare, TLS can also occur spontaneously before any treatment is initiated 🤯.
How does treating a cancer cause a potentially life-threatening event? Isn’t the goal of cancer treatment to kill the cancer cells and stop the spread of disease? Yes, you are correct.
(Image)
However, when we kill (or “lyse”) a large number of tumor cells at one time and these cells spill all of their contents into the bloodstream, the body can quickly become overwhelmed (similar to the brain after reading a Phase I clinical trial protocol). This series of events causes the ‘syndrome’ of TLS.
Michael Scott is also confused. You’re not alone. (Image)
Now, let’s take a step back for a moment. A “syndrome” is a big word for a group of symptoms, which is different than a “disease” which causes organ dysfunction with specific signs and symptoms. For example, irritable bowel syndrome (IBS) is characterized by symptoms such as abdominal pain, bloating, diarrhea, and constipation. Each of these symptoms alone does not point to IBS, but as a collection they may uncover a possible cause. Still confused? Hang in there!
(Image)
Back to your scheduled programming. Let’s set the scene. Your patient has just been diagnosed with lymphoma, a cancer of the lymphatic system (basically the gutter of the body). The team begins an effective treatment that immediately starts to barge through the cancer cell walls like Gerard Butler busting through a wall of soldiers in the film 300.
When the flood gates open, the contents of these cancer cells dump into the bloodstream. You may be asking yourself, what are the cellular contents being spilled?
Another great question! The biggest players to consider here are potassium, phosphorous, and nucleic acids.
Why does it matter that a patient’s blood now has more potassium, phosphorus, and nucleic acids? These don’t sound that bad, and the doctor always suggests getting more potassium in my diet (bananas!).
Well, the rapid increase of these cellular contents in the bloodstream can cause a variety of problems, such as renal dysfunction (you know, that vital organ that works like a horse to filter out your blood), cardiac arrhythmias, seizures, neurologic complications, and death. When electrolytes exceed the upper limit of normal (ULN), they can have negative effects on your body, such as hyperkalemia causing muscle weakness, nausea, and cardiac arrhythmias.
FYI, a good way to remember that potassium is cardiotoxic is knowing that it has been included as part of many states’ lethal injection execution protocols.
And we continue!
Hyperphosphatemia can lead to secondary hypocalcemia (these two are like long-lost lovers and bind to each other like a panda on bamboo) which can cause bone and muscle problems, seizures, and also cardiac arrhythmias. As you can see, the heart could potentially have a very bad day if TLS is not prevented.
This bean is happy to be taken care of. (Image)
Last, but certainly not least, the breakdown of nucleic acids is facilitated by xanthine oxidase. This enzyme efficiently converts nucleic acids into hypoxanthine, then xanthine, and finally uric acid. Unfortunately, having too much uric acid (hyperuricemia) can cause your urine, and rarely blood, to become acidic. Supersaturated urine can promote formation of uric acid crystals that become too big for the kidneys to filter, which doesn’t lead to anything good – take care of the beans!
Who is at Risk for TLS?
Now that you are interested and invested in becoming a TLS life saver (you’re invested, right?!), whom do you need to protect?
CK is ready to be a TLS life saver too. (Image)
Remember, TLS occurs most frequently in people with cancer in the blood, such as leukemias and lymphomas; however, more recently this emergency has been reported in cancers not in the blood, such as uterine and kidney cancers. So TLS should really be on your radar for any patient with cancer.
As if having cancer wasn’t bad enough, TLS is just one of many toxicities patients can experience that pharmacists need to assess. To understand the likelihood of TLS in any given patient, there are risk factors to consider. These are grouped into patient, treatment, and cancer-specific factors:
TLS has historically been associated with cytotoxic treatments (those that quickly kill a cell). With the use of more novel and targeted agents, we are discovering these traditionally cytostatic drugs can cause TLS too. Another reason why oncology is a great specialty for pharmacists – who else can keep up with the revolving door of drug data?!
(Image)
Despite knowing which drugs and cancers are most commonly associated with TLS, there are exceptions to every rule. Although most solid tumors are considered low risk, there are some persnickety ones that are highly sensitive to treatment and are classified as intermediate risk. These include neuroblastoma, germ cell tumors, and small cell lung cancer.
Can We Prevent TLS?
Since we can identify who is at risk, we should be able to prevent this party crasher, right? The answer is yes!
There are 2 simple steps to help decrease, and hopefully eliminate, the chance of TLS occurring:
Hydration – this is KEY! Hydrating a patient before treatment keeps fluid moving through the kidneys so they can filter the increased electrolytes and to minimize acidosis (the cheerleader for uric acid crystal formation).
A typical hydration order is 2,500-3,000 mL/m2/day normal saline 2-3 days before, during, and 2-3 days following treatment - I know, it’s a lot of fluids for days on end, but it’s for a good cause!
If urine output is not increasing with fluids alone, diuretics may be given.
Drug prophylaxis – allopurinol, febuxostat, and rasburicase are all pre-medication options to minimize hyperuricemia and prevent the formation of uric acid crystals. Allopurinol and febuxostat help prevent formation of uric acid, while rasburicase lowers uric acid levels directly.
Allopurinol is administered orally (unless critically ill) 1-2 days before, during, and 7-14 days after treatment and is the standard prevention medication.
In clinical practice, 300 mg PO daily is the most common dosing.
Febuxostat is an alternative to allopurinol and is administered similarly.
In clinical trials, 40-120 mg PO daily was used.
Rasburicase is rarely used in the prophylaxis setting due to cost ($$$) except in patients with rapidly increasing blast counts, high uric acid at treatment initiation, or renal dysfunction.
For those visual learners, the graphic here shows how these drugs act in the nucleic acid breakdown pathway. Remember, allopurinol and febuxostat prevent the formation of uric acid, and rasburicase speeds up its conversion into allantoin, which is more soluble than uric acid and allows it to be excreted. (We’re not talking about probenecid here, just ignore that arm). (Image)
FUN FACT: Uric acid blood samples that are drawn after rasburicase is administered (for ongoing monitoring) must be transported to the lab on ice. This is because rasburicase quickly binds uric acid and can cause falsely low readings on the way to the lab!
Your patient’s blood sample heading to the lab. (Image)
How Do You Know If Your Patient Has TLS?
After assessing a patient’s risk and initiating preventative measures, your patient begins showing signs that you suspect could be TLS. How can you be sure? Luckily, there are published classification criteria that define the 2 types of TLS we see: laboratory and clinical TLS.
The Cairo/Bishop criteria was introduced first and is more broad than the Howard criteria but they are fairly similar:
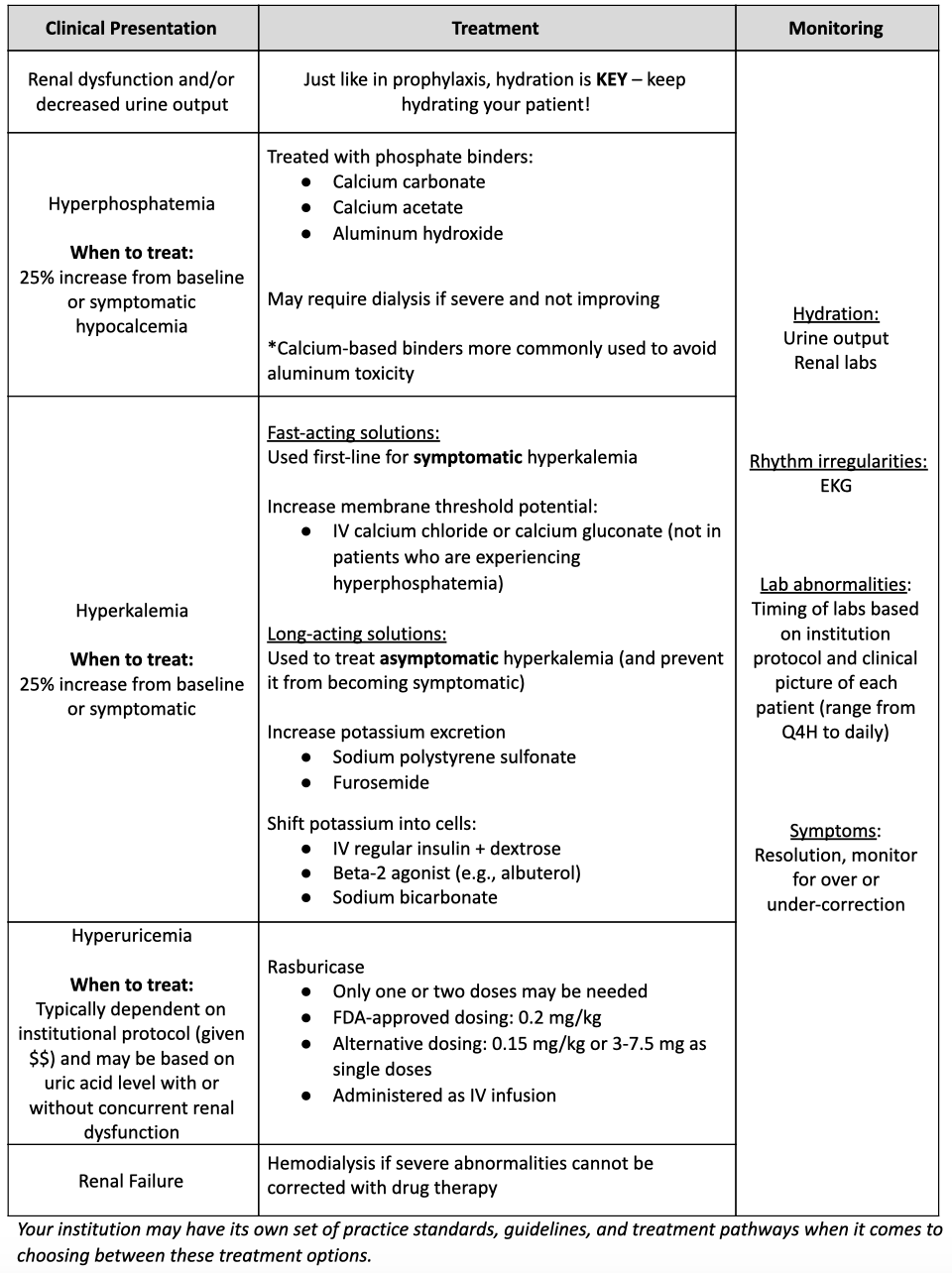
Your Patient Has TLS – Now What?
(Image)
Don’t panic! Although you have checked off all the prevention boxes, your patient may still experience TLS. The good news here is that you recognized it (by knowing the syndrome), and it is reversible with correct treatments! Here is how you can manage TLS:
The Value of the Pharmacist in TLS
Pharmacists play a vital role in the prevention and treatment of TLS. We see medications through a very specific lens which enables us to identify, prevent, and resolve medication-related issues. When helping manage oncology patients, pharmacists can:
Identify high risk treatment regimens
Educate the team on monitoring parameters
Make patient-specific prevention and treatment recommendations
Be a drug information resource
Since everyone loves clinical pearls (I mean, really, who doesn’t?!), here are some important ones every pharmacist should know regarding allopurinol and rasburicase, the 2 big players in TLS management!
Allopurinol
Renally-cleared so may require dose adjustments
Common adverse drug reactions (ADRs) include skin rashes (including Stevens-Johnson syndrome, etc.) or other allergic reactions
Many drug interactions in the oncology population including: capecitabine, mercaptopurine, azathioprine, aluminum hydroxide, and warfarin
In TLS treatment, consider starting after rasburicase is given to prevent formation of NEW uric acid (will not lower current levels!)
Do NOT give concurrently with rasburicase
Rasburicase
Common ADRs include peripheral edema, headache, fever, nausea, and vomiting
Contraindicated in those with G6PD deficiency - those patients can receive allopurinol
Can cause hypersensitivities with repeated exposure
Congratulations, you did it! Now you are informed and ready to identify, prevent, and manage tumor lysis syndrome. Go make a difference in your patients’ lives!
Also, if this content has sparked your interest in oncology, get support at www.KelleyCPharmD.com.
(Image)
BTW - We compiled ALL of our Oncology Supportive Care posts into one handy, downloadable (and printer-friendly) PDF. You can get your copy of it here.