Acute Stabilization of Severe Bleeds Part 3: Gastrointestinal Bleeds
Steph’s Note: Welcome back to the last post of our three-part series. In Part 1, we talked about anticoagulation reversal in patients with acute severe/life-threatening bleeds. In Part 2, we shifted our focus to the acute management of traumatic brain injuries/intracranial hemorrhages. And now, we’ll finish off the series with Part 3, in which we will talk about the management of gastrointestinal and variceal bleeds. Here to teach us is Gabrielle, who worked with our critical care guru, Dr. Josef Nissan, on rotation.
Gabrielle is a current P4 at Lipscomb University College of Pharmacy in Nashville, Tennessee. She's interested in applying for an acute care PGY1 residency to further specialize in critical care as a PGY2. Her critical care interests include trauma, cardiology, and traumatic brain injury. Aside from pharmacy, she enjoys hiking, cooking, and volunteering at a local animal shelter walking and fostering dogs. She's also trying to learn how to make a starter feed for baking sourdough bread -- so if you have any tips, send them her way!
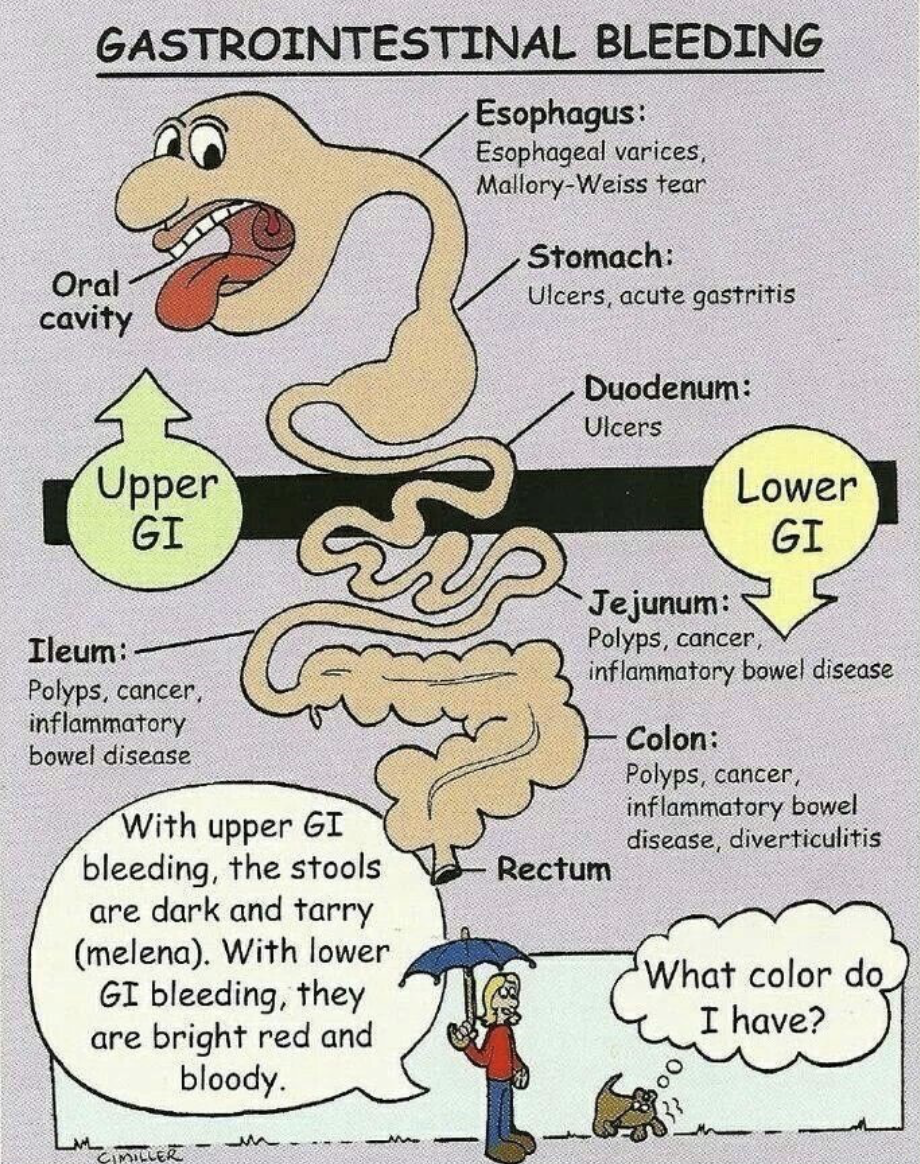
GI bleeds at a glance… more details to come. (Image)
Gastrointestinal (GI) bleeds. Two words that have been jammed into our heads throughout pharmacy school. Non-steroidal anti-inflammatory drug (NSAID)-induced, diverticular, and variceal bleeds – Oh my!! Treating GI bleeds as an emergency is crucial as things can get messy – fast! No pun intended.
Treatments for a GI bleed depend on the location of the bleed (upper versus lower bleeds), unique pathophysiology, and patient factors. Now, before we get into the treatments, let’s get reacquainted with the different types of GI bleeds by divvying them up into upper GI, lower GI, and variceal bleeds.
What is an Upper Gastrointestinal Bleed?
The upper gastrointestinal tract starts with the esophagus, leads to the stomach, and ends with the first part of the small intestine called the duodenum. Sounds easy enough, right? What could ever go wrong? Well...
Peptic ulcers
Ulcerations in the GI tract in the setting of increased susceptibility to gastric acid and decreased protective mechanisms
Erosive esophagitis
Esophageal mucosal injury caused by gastrointestinal reflux
Gastritis
Diffuse inflammation of the stomach lining
Mallory-Weiss tears
A tear in the lower esophagus caused by intense coughing or vomiting
Yep, that’s right, folks. You actually CAN vomit so violently that you tear your poor GI tract. Eepers. (Image)
Peptic ulcer disease (PUD) wins the superlative for most likely to cause a GI bleed and the one we’ll learn more in-depth.
PUD and Upper GI Bleeds
PUD causes more than 50% of all upper GI bleeds. When the mucosal lining has decreased protective mechanisms, such as reduced prostaglandin synthesis and bicarbonate secretion, and increased permeability to stomach acid, it can lead to problems in the outer lining of the GI tract. PUD ulcerations occur more in the stomach and duodenum than in other parts of the digestive tract.
What increases the risk of PUD? Well, I’m glad you asked!
The most common risk factors are H. pylori, NSAID use, critical illness (sepsis, trauma, burns, mechanical ventilation), and high-dose corticosteroids.
H. pylori in the illustrated flesh. Ughhhhh. Eradicate that junk, yo! (Image)
Helicobacter pylori is a bacteria that thrives in acidic environments and causes direct insult to the gastric lining, leading to inflammation and breakdown of the mucosa, further resulting in ulcers. (Interestingly, this bacteria has actually been designated as a human carcinogen for its role in gastric cancer.)
NSAIDs decrease prostaglandin synthesis, which normally helps to protect the mucosal lining.
Then there’s the whole bucket of stress-induced ulcers caused by critical illness! Stress-induced ulcers come into play in the setting of mechanical ventilation, clotting abnormalities, trauma, and many others when blood flow to the gastric mucosa is reduced.
So now that we have that down... How do ulcerations or breakdown of the GI mucosa cause bleeding?
Small blood vessels are embedded in the mucosal lining, which gets blood from arterioles from the submucosa (the layer beneath the lining). Depending on the degree of ulceration, the bleeding can occur within the small vessels in the upper lining... or the tear may start to extend into the submucosa, and the larger vessels can let out a massive bleed. (cue the doors from The Shining) Hence... GI bleeds are a medical emergency!
What is a Lower Gastrointestinal Bleed?
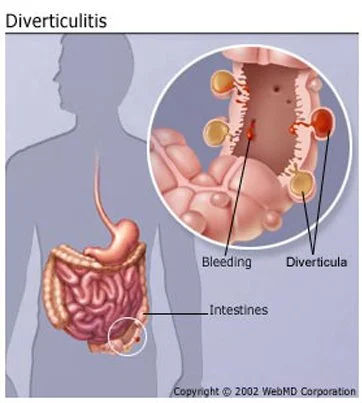
See the pouches? Those are diverticula, and they can encroach on blood vessels, leading to bleeding. (Image)
Now that we have the upper GI part down, let’s get our hands dirty with the lower GI tract. Again, no pun intended.
The lower GI tract consists of the rest of the small intestine (jejunum and ileum), the large intestine, the rectum, and the anus. Lower GI bleeds typically are of lower severity and have lower fatality rates. Common instigators of lower GI bleeds are:
Diverticulosis
Small pouches that form in the small and large intestines are commonly present with increased age. Diverticula are most likely present in the sigmoid colon, where blood vessels protrude into the mucosal layers. Mucosal layers are more prone to injury, leading to bleeding into the stool.
NSAIDs
Yup, this one again.
Angiodysplasia
Abnormal swollen blood vessels that are localized in the GI tract (more common in the colon) and are prone to bleeding.
Inflammatory causes
Infection or inflammatory bowel disease (Crohn’s disease or ulcerative colitis), where chronic inflammation leads to ulceration in the lower GI tract.
Bowel movement straining
Veins around the anus become swollen due to increased localized pressure, leading to hemorrhoids. A tear in the lining of the anus can also occur and lead to anal fissures.
What is a Variceal Bleed?
Variceal bleeding is a type of upper GI bleeding with a totally different underlying cause. It is typically seen in cirrhotic patients.
When cirrhosis occurs, blood flowing through the portal vein becomes obstructed, pressure in the portal system rises, and blood is diverted to other systemic veins. One area where the blood is shunted is the esophagus. And because our body is magnificent and can adapt to changes, we begin to develop other routes to get blood to the esophagus.
Thus, we develop esophageal varices. These varices (aka enlarged veins) are very fragile and cannot handle a large amount of blood like the rest of our vasculature. As a result, they are prone to rupturing and can lead to life-threatening variceal bleeds. Make sense? Kind of? Ok let me simplify it even further.
Let’s say you have a large 4-lane highway (aka the portal vein) that goes to New York City (aka the esophagus). Now let’s say there's a really bad accident (aka advanced liver disease) on this large 4-lane highway, which blocks entry into New York City (aka the esophagus). Well, people still need to get to New York City, so naturally, everyone will divert to driving on small backroads (aka esophageal varices). These one-lane backroads are very small and can’t handle a lot of traffic. As a result, they are prone to more accidents (aka variceal rupture and bleeding).
Now does it make sense? Ok, good.
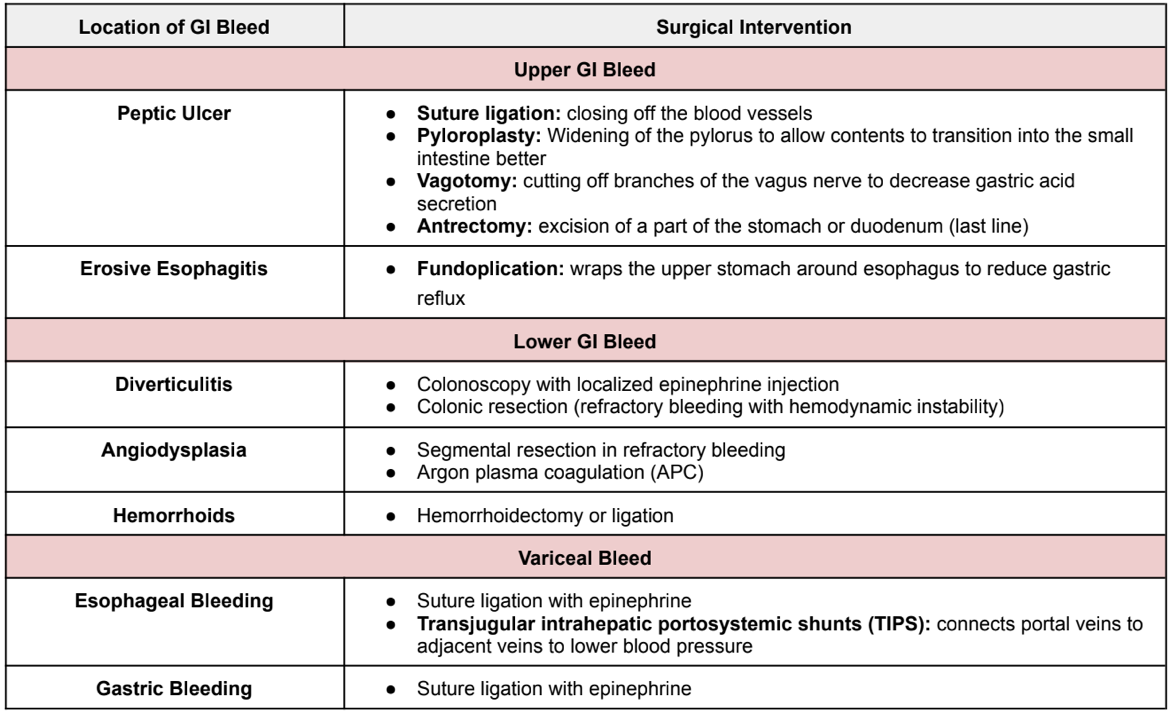
Gastrointestinal Bleed Management - Surgical Interventions
I know we’re not surgeons here... but some of these bleeds have treatments other than the use of good ol’ drugs. GI physicians and surgeons can deliver surgical or localized treatments to stop bleeding during an endoscopy or colonoscopy.
However, if the source of the bleed cannot be found or continuous blood loss occurs, further surgical intervention is required. Here is a handy dandy table that gives you a basic summary of the common surgical interventions that can be made:
Gastrointestinal Bleed Management - Pharmacologic Interventions
Now, let’s get to our favorite part! The drugs!
Luckily, treatment for most GI bleeds tends to be similar, with slight nuances between disease states. Before we take a deep dive into the agents targeting the GI tract, we need to assess the patient’s hemodynamic status. Is the patient hypotensive? Does the patient need a blood transfusion?
Maintaining Hemodynamic Stability
Patients experiencing GI bleeds can have large amounts of blood loss, so keeping them hemodynamically stable is crucial. If possible, patients should be hemodynamically stable before endoscopy or colonoscopy. Here are some pearls for hemodynamically unstable patients with a GI bleed:
ABCs: Making sure the patient can breathe (intubation) if they cannot maintain their airway and blood pressure.
Fluid resuscitation: Fluid resuscitation should be started immediately for hemodynamically unstable patients (500 mL of lactated ringer or normal saline).
Transfusion: Packed red blood cells should be given to patients who have a hemoglobin <7 g/dL.
Assessed hemodynamic stability? Check! Let’s treat some bleeds.
Acute Treatment of Upper GI Bleeds
Treatments for general upper GI bleeds have a common theme. Please welcome the star of the show, the proton pump inhibitor (PPI).
First-line Treatment: Pantoprazole (Esomeprazole also comes in IV formulation with equivalent dosing)
Continuous infusion (IV): 80 mg bolus, followed by 8 mg/hr until endoscopy with subsequent dosing based on endoscopic findings.
Intermittent dosing (IV): 80 mg once, followed by 40 mg every 12 hours until endoscopy. Subsequent dosing is based on endoscopic findings.
So then, which should we recommend? Continuous infusion or intermittent dosing?
I’m so glad you asked because this is a topic that I get overly passionate about. Yes, guidelines generally recommend continuous infusion dosing. HOWEVER, primary literature has yet to show any increased efficacy with continuous infusion dosing. There are so many meta-analyses that have been completed to prove this. Time and time again, studies show that there is no significant difference between continuous infusion and intermittent dosing in regards to rebleeding, need for urgent intervention, mortality, red blood cell transfusion, and length of hospital stay. However, intermittent dosing provides a smaller daily dose, is much easier to administer, and costs less.
So the clear winner here is.........INTERMITTENT PPI DOSING. Thanks for coming to my TED talk.
Acute Treatment of GI Bleed in the Setting of H. Pylori
Testing for H. pylori occurs when ulcers are present in the stomach or duodenum. If the test is positive, we gotta treat the bug to reduce the risk of further ulcerations and bleeding.
First-line Treatment: Bismuth Quadruple Therapy
PPI: Any PPI will do. The patient will already receive one in cases of active upper GI bleeds.
Bismuth subsalicylate 525 mg PO four times daily (spearmint anyone??)
Metronidazole 250-500 mg PO four times daily
Tetracycline 500 mg PO four times daily.
This regimen takes first place in the context of penicillin allergy and prior macrolide usage.
Second-line Treatment: Clarithromycin Triple Therapy (Oral clarithromycin triple therapy is suitable for low clarithromycin resistance (<15%) and no prior macrolide usage. Pill burden is less of a concern in triple therapy since treatments are given two or three times daily compared to four times daily in quadruple therapy.)
PPI
Clarithromycin 500 mg PO twice daily
Amoxicillin 1 g PO twice daily or metronidazole 500 mg PO three times daily
Acute Treatment of NSAID-induced GI Bleeds
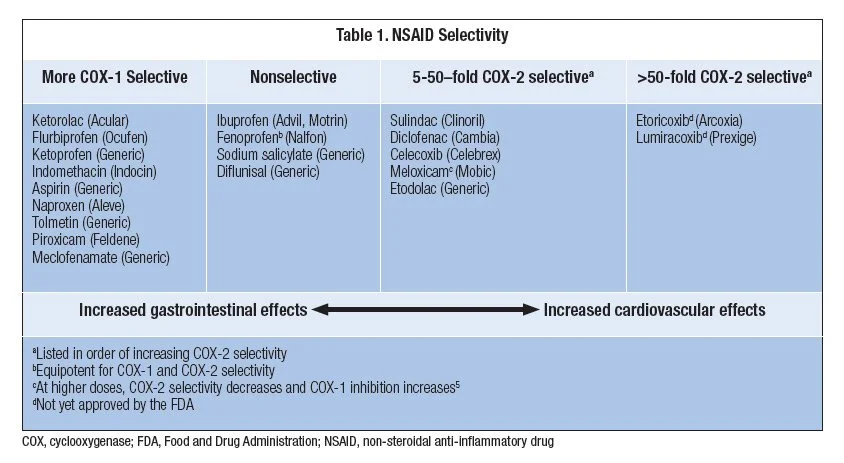
Ah, cyclooxygenase – we meet again. NSAIDs work by inhibiting an enzyme called cyclooxygenase (COX), which has two types: COX-1 and COX-2. Inhibition of COX enzymes by NSAIDs reduces prostaglandin synthesis. Prostaglandins protect the GI mucosal lining, which means NSAIDs basically assassinate this natural protection.
That being said, the GI tract heavily expresses COX-1, which has prominent platelet-activating effects. Inhibition of COX-1 increases the risk of gastric ulceration and bleeding. COX-2 selective NSAIDs don’t utilize the COX-1 pathway as much, leading to reduced risks of GI bleeding.
For NSAID-induced gastric bleeding, you can do one of two things:
DISCONTINUE THE NSAID (this is always preferred), or
Switch to a COX-2 Selective NSAID (etodolac, celecoxib, nabumetone, meloxicam, diclofenac)
Well THIS is useful! (Image)
In cases where NSAIDs must be kept on board despite evidence of ulceration and bleeding, low-dose misoprostol is used for mucosal prostaglandin protection.
Acute Treatment of Lower GI Bleeds
Most cases of lower GI bleeding are either managed through surgery during colonoscopy or resolve spontaneously. PPIs are not recommended to treat lower GI bleeds as they only inhibit acid production in the stomach (i.e., upper GI tract).
Medications to treat underlying disease states (irritable bowel disease, constipation, etc.) should be utilized. Also, NSAIDs can be discontinued or replaced with COX-2 selective inhibitors (if previously non-selective) to decrease the risk of lower GI bleeding. Over-the-counter medications, such as Preparation H (phenylephrine) ointment, can be used to treat hemorrhoids. Preparation H reduces the swelling in the affected area by constricting the blood vessels.
Acute Treatment of Variceal Bleeds
The acute treatment of variceal bleeding focuses on reducing blood flow to the GI tract and antibiotic prophylaxis.
Blood Flow Reduction
First-line Treatment: Octreotide 50 mcg IV bolus followed by a continuous infusion of 50 mcg/hour for 2-5 days
Antibiotic Prophylaxis
Patients with cirrhosis who experience variceal bleeding are prone to developing spontaneous bacterial peritonitis (SBP). Third-generation cephalosporins are preferred for prophylaxis as gram-negative bacteria commonly cause SBP. In cases of active variceal bleeding, antibiotics reduce mortality and risk of re-bleeding.
First-line Treatment: Ceftriaxone 1 g every 24 hours for 7 days
Patients with a history of variceal bleeding are at high risk of recurrence, which makes secondary prophylaxis essential. Non-selective beta blockers lower portal vein pressures by inducing splanchnic vasoconstriction, thereby decreasing bleeding risk. (I know…if you’re thinking to yourself, “Whaaaaat? Beta blockers cause vasoconstriction???”, you’re not alone. Check out this post on variceal bleeding for a more detailed explanation!)
First-line Treatment: Non-selective Beta Blockers*
Propranolol 20-40 mg twice daily
Nadolol 20-40 mg once daily
Carvedilol 6.25 mg once daily, can increase to twice daily after three days
*Starting doses are given; doses can be titrated every 2-3 days to the maximum suggested dose or frequency, systolic blood pressure, heart rate, or prevalence of ascites.
Tl;dr of Gastrointestinal Bleeds
GI bleeds can occur in either the upper GI tract (esophagus, stomach, and duodenum) or the lower GI tract (jejunum, ileum, large intestine, rectum, and anus). Common causes of upper GI bleeds include peptic ulcers (most common cause), erosive esophagitis, and Mallory-Weiss tears. Common causes of lower GI Bleeds include diverticulosis, NSAIDs, angiodysplasia, inflammation, and straining during a bowel movement. Variceal bleeding is a type of upper GI bleeding with a totally different underlying cause and is typically seen in cirrhotic patients.
Surgical treatments can be used to manage the bleeding in combination with endoscopy or colonoscopy. Resection of bowels is indicated in patients with continuous bleeding, leading to hemodynamic instability despite prior treatments. Initial treatment of GI bleeds focuses on hemodynamic stability with fluid resuscitation and transfusion if hemoglobin is less than 7 g/dL.
IV proton pump inhibitors are the mainstay of treatment for acute upper GI bleeds, and if H. pylori is detected, treatment with quadruple bismuth antibiotic therapy or clarithromycin triple therapy is recommended. Most lower GI bleeds are treated surgically or will generally resolve on their own. Regardless of the location, NSAIDs should be discontinued or switched to COX-2 selective inhibitors in the setting of GI bleeding.
For variceal bleeds, use of octreotide to shunt the splanchnic circulation remains the treatment of choice for varcieal bleeds until surgical interventions can be made. Patients with variceal bleeding are prone to SBP and are started on ceftriaxone prophylaxis for 7 days. Non-selective beta blockers may be employed to decrease the risk of variceal re-bleeding.